Deja Vu. Data- Driven Retail Strategies, For Health Care This Time
 April 9, 2012
April 9, 2012 
Health care companies today are following in the footsteps of the retail-oriented, information based financial services industry.
What financial services companies have discovered is that in order to build their business, they must build a personal relationship with the consumer. They accomplished this by creating a consumer-centric database, monitoring shopping behavior through reporting and analytics, motivating activity through multi-channel communications and launching a loyalty program to reward consumer spending,
I was part of this customer-centric transformation as the Director of Database Marketing at GE Capital, which provides private label credit card programs for Disney and Apple, to name a few marquee brands. My cross- functional team started with the consumer in mind. We envisioned the experience that our retailer customers needed to deliver to their consumer card holders to differentiate themselves in the marketplace and capture a larger mind share and business share.
This is the same path that health care companies are marching down to get ready for new customers.
Consumers Are Coming! Health Care Companies Invest in Retail Strategies
In their report on “The Era of the Health care Consumer,” Accenture describes the shift in responsibility from the employers to the consumers and the resulting health care company investment changes from BTB to BTC. Accenture cites the opportunity to learn from the retail sector, especially the segmentation, profiling, loyalty and cross channel communications.
A few health care organizations are making the needed investments to move closer to the consumer in order to better understand their needs for information and tools to support health management. Aetna, for example, has partnered with Best Buy to sell wellness programs to consumers within the retail store and deliver their wellness coaching program online. In addition to store fronts, Florida Blue (previously BCBS Florida) has invested in their Guidewell online initiative to build a relationship with consumers beyond their member base.
Most health care companies, however, are still trying to figure out where to begin.
Barriers for Data-Driven Retail Health Care
There are several key barriers that Health care companies must overcome in order to effectively engage these retail consumers.
- Knowledge about the New Consumer: Health care companies have limited or no information about their newest customer that is either considering their health product/service or has just come onboard. As a result, the interaction can feel less satisfying. Using best practices from the financial industry, health care organizations can utilize segmentation and profiling to deliver a more personalized experience while gathering knowledge about the consumer through each touch.
- Knowledge about Consumers' Data Needs: During their recent research, IDC Health Insights learned that “despite large investments meant to extend the organizations’ consumer-centric model, health plans know little about how consumers want to consume information…”. Financial Services companies remain aligned with their customers by inviting them to participate in their own private branded online research community. The company captures consumer input and feedback on their product road map and new marketing initiatives.
- Knowledge about Proactive & Personalized Communications: Many health care organizations wait for consumers to come to their online marketing destinations including their website and social media and then wait for them to return. Although these companies maybe have tools in place to capture the contact information of interested consumers, they tend to send out the same information to everyone. Financial Services companies segment these target consumers and stream content of interest across their preferred communication channels to bring them back and engage.
- Knowledge about Developing a Personalized Incentive Program: One way that health care companies can differentiate themselves is with an incentive program that rewards a consumer for healthy lifestyle behaviors that fit her profile. One of the reasons that some credit card loyalty programs (e.g. American Express) are so effective is that they target personalized offers based on each consumer’s spending behavior profile.
Health care companies can learn from the leaders in the Financial Services industry about how to leverage technology to build a retail consumer relationship through ongoing personalized communications and programs which are aligned with the consumer’s ongoing data needs.
Connected Mobile Health Apps to Sustain Consumer Engagement
 March 30, 2012
March 30, 2012  World Congress Leadership Summit on Mobile Health, July 25-27th in Boston
World Congress Leadership Summit on Mobile Health, July 25-27th in Boston
Over the past three years, I have participated in this interesting event by running a workshop or panel.
- Connecting multiple mobile apps to personalize the care shopping, decision making and care collaboration experience.
- Connecting mobile into chronic care programs with integrated tools for self management, shared decision making and coaching support.
- Connecting mobile into wellness programs with capabilities to harness social community influence, digital coaching and incentives for motivation.
- Dan Brostek, Head of Member and Consumer Engagement, Aetna
- Michael Yetter, Director, eBusiness, Independence Blue Cross
- Nick Martin, VP Innovation and R&D, UnitedHealth Group
- Patrick Feeney, Director, Mobile and Emerging Technologies, Blue Cross Blue Shield Illinois
UnitedHealth Group Integrates Multiple Mobile Apps for Holistic Self Management & Coaching
 March 8, 2012
March 8, 2012  Health Plans are finding new ways to bring value to consumers by empowering them with tools and guidance to manage their health while on the go.
Health Plans are finding new ways to bring value to consumers by empowering them with tools and guidance to manage their health while on the go.
At many conferences, health plans present their newest mobile application or texting campaign to engage consumers.
UnitedHealth Group announced their latest move at the recent Consumer Electronics Show to integrate several mobile health applications into their OptumizeMe solution, through partnerships with CareSpeak Communications, FitNow and FitBit. UnitedHealth is integrating content and tools to bring new capabilities to both consumers and caregivers.
Through the CareSpeak Communications’ partnership, consumers sign up to receive two-way texts to help them manage their medication and condition. UnitedHealth delivers CareSpeak’s personalized messaging to provide relevant content to each consumer segment ( e.g. asthma, diabetes, cancer, etc). A patient with diabetes opts in to receive customized education and reminder messages and can give a caregiver permission to monitor her health. The patient’s clinician is also kept in the loop with medication and condition management data to discuss during patient interactions. Patients are further engaged by receiving text based educational quizzes and viewing online reporting showing their effectiveness in managing their medication and condition over time.
With the integration of FitNow’s Lose It! mobile app, consumers can better manage their weight through fitness and food tracking tools, educational nutrition information, motivational reminders and social peer support.
From the FitBit integration, consumers automatically track their physical activity instead of having to key it in. Since this activity data is no longer self reported, UnitedHealth Group can use validated information to drive their rewards program. The FitBit app also tracks the consumer’s sleeping behavior for a more complete view of their health.
Integration Delivers Insight
UnitedHealth Group has invested in this set of mobile technologies to capture and connect multiple sources of data for a holistic view covering the consumer’s physical activity, dietary behavior, medication adherence, biometric and mood information.
“With these partnerships in place, we are connecting all the pieces of data across our platform for a common view for the consumer to self manage and share with their coach while creating a personalized experience”, explains Nick Martin, VP Innovation and R&D, UnitedHealth Group.
This supports the trend for “integrated end to end health to care solutions” where technology connects with care management platforms and programs, as noted by IDC Health Insights’ analyst Janice Young.
Coach/CareGiver & Consumer Collaboration
Nick Martin describes how the OptumizeMe application is being used by the consumer with their coach. “Let’s say you are trying to lose weight. Your coach can push messages to your mobile which are educational and supportive. And if you give your coach permission, she can see your tracked physical activity”. Think about how much more motivated and accountable the consumer will feel when her coach is monitoring and responding to her daily progress. On the health side, the asthma patient can give access to her caregiver to monitor and address medication compliance issues. Her caregiver can also send encouraging and educational messages between visits.
UnitedHealth’s partnerships deliver new capabilities to their OptumizeMe mobile app giving consumers a new way to remain in close contact with their coach and to self manage with the social support from caregivers. With the power of the personalized information pushed and pulled from the consumer’s mobile phone, UnitedHealth Group can successfully generate both stronger consumer engagement and better health outcomes.
 educating consumers about health and wellness,
educating consumers about health and wellness,  mobile health and wellness texting,
mobile health and wellness texting,  mobile health application,
mobile health application,  online health and wellness coaching,
online health and wellness coaching,  self- management health tools in
self- management health tools in  Behavior Change Health & Wellness,
Behavior Change Health & Wellness,  Data Driven Health Engagement,
Data Driven Health Engagement,  Decision Support eHealth,
Decision Support eHealth,  Mobile Engagement Health & Wellness
Mobile Engagement Health & Wellness Regence Reaches Step 3 on their Consumer Engagement Path
 February 14, 2012
February 14, 2012  Regence Program Rewards Transformational Activities
Regence Program Rewards Transformational Activities
Regence started on a new path to consumer engagement back in 2005.
After seeing a recent presentation outlining their consumer engagement framework, I reached out to Torben Nielsen, VP, eBusiness Strategies and Services at Regence to learn more. Torben shared their past journey as well as their future direction with me.
Here are the 4 steps along their consumer engagement path. Regence is currently at Step 3 and has a conceptual view of their next step which will continue to evolve as the market landscape fills in around them.
Consumer Engagement Step 1: Know Me
Regence’s first step focused on the passive cardholder, giving them value as they logged in. The cardholder saw all of their claims, benefits and provider information. This was back in 2005. Prior to that “it was not a good experience” since the member only saw some of their claims information and the list of providers “did not even indicate whether each one was inside or outside their network”.
Consumer Engagement Step 2: Engage Me
Beginning in 2008, Regence decided that they needed to get to know their members in order to effectively engage them.
Instead of linking the member over to their health or wellness program vendor’s website, Regence decided to keep the member within their portal to capture their online behavior.
Around that time, Regence launched their Rewards Program which awarded points to members for “tranformational activities”. These activities were rewarded because they “informed, empowered and educated the consumer”, including looking up content around a health issue or participating in a wellness program. Regence decided not to reward members for “transactional activities” such as looking up a claim or searching for a provider. Regence really needed to keep the member on their portal to track their online behavior in order to reward them.
Next Regence started their email program, sending out relevant electronic communications to bring members back to the site. Although many health plans have an interest in emailing members, I hear all the time that they do not have their email addresses. Regence collects the member’s email address during their site registration process. “We can’t engage with out email. It would be a missed opportunity to get in front of the member”, Torben emphasizes.
In addition to generating additional portal traffic, health plan communications can also strengthen their member’s satisfaction scores, which is more important now than ever with the increased market competition.
Consumer Engagement Step 3: Connect Me
Over the past two to three years, Regence has been moving faster down the path with consumers.
“Connect Me” goes beyond the “member to health plan” relationship. According to Regence, this also includes strengthening the “member to member” bond through social community and the "member to their care team" bond through ACO efforts.
One important way for Regence to strengthen the “member to member” relationship is by getting consumers to contribute more content online through conversations, ratings/reviews and suggesting local events in their geography.
Another aspect of “Connect Me” addresses the cross communication channel experience since members are increasingly accessing and engaging through their mobile devices. “We’re connecting the data that we’re sitting on to provide a more personalized experience for our members”, explains Torben.
Consumers are engaging with Regence!
- 67,000+ patient reviews have been submitted by members, of which 90% are favorable (i.e. the member would recommend the physician/facility).
- 63,000+ posts in the Community section of myRegence.com, written by more than 6,000 unique content creators.
- 346,000+ have opted- in for member electronic communications (e.g. updates and alerts, account information, etc)
- 260,000+ subscribers signed up to receive the bi-weekly myRegence.com email newsletter
Consumer Engagement Step 4: Partner with Me
As they look down their Consumer Engagement path, Regence has determined where they want to be directionally. Regence wants to be relevant to the consumer’s every day life. Something consumers need to check as part of their daily routine. Their starting place to look for information to meet all of their health needs.
Although it is challenging to know exactly where the market is going, Regence will remain in touch with their users to help guide the way.
In fact, Regence has over 400 users that help advise them by providing ongoing feedback to potential directions. [Note: Innovative companies have consumer advisory boards as a best practice. Increasingly, these consumer advisory boards are managed in a private online area and the insight captured is used to guide product and marketing decisions.]
Regence is co-creating with this growing group of consumers to define and refine online capabilities. When Regence asked for feedback about “patient reviews”, members felt they needed to see more than the reviewer’s screen name. Users wanted “the ability to connect with their peers in order to get advice when selecting a provider”. In the latest patient review experience, the screen name is linked to the reviewer’s Community profile page, where to learn more about who they are, where they’re from, what they do for a living and members have an the opportunity to make a friend request.
Regence’s Results Realized
Due in large part to Regence’s consumer engagement strategies, myRegence.com experienced the following results in 2011 over 2010:
- 30% increase in the cumulative number of content creators (i.e. those who have left a patient review, posted in Community or both).
- 88% jump in the number of $25 gift card redemptions through the Rewards program
- 76% increase in the Consumer Engagement Index (CEI) which measures the user adoption of transformational features
- 26% open rate for targeted email campaigns, nearly 2x the industry benchmark of 14%
Regence has also noticed that their segmentation efforts for email have been effective in engaging consumers. For example, by sending a Patient Review email to previous reviewers, Regence realized a 38% open rate.
As Regence moves onto step 4 in Consumer Engagement, they are conceptualizing new ways to reach out to their members with relevant information from their plan, community and care team. And they will be innovating with and listening to their users throughout their journey.
Shared Decision Making Tools Engage Consumers for Better Outcomes and a Better Experience
 September 27, 2011
September 27, 2011 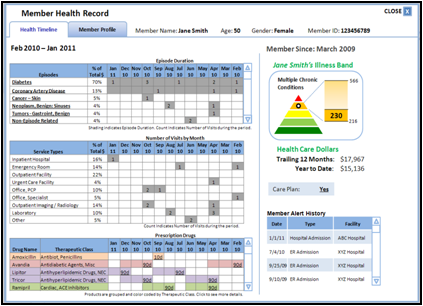 CareFirst BCBS Medical Home SDM Tool
CareFirst BCBS Medical Home SDM Tool
Over two years ago, I led a panel on patient decision support tools for a large interested crowd in Boston, despite the very snowy day.
Since then, I have noticed a few key changes. Physicians are now prescribing information to patients, using the EMR to send emails with links to health resources. And innovative health plans are playing a role in bringing shared decision making tools to engage and empower their members. Health Plans have a big cost saving incentive when these tools educate their members about less invasive and less expensive options.
3 Key Engagement Drivers With Shared Decision Making Tools
While evaluating technologies for my panel on “Evolving Web & Mobile Tools to Engage Consumers in the Shared Decision Process”, I identified how three key drivers of consumer engagement are being utilized:
1. Education
These tools show the consumer what the treatment entails and share patient stories which tell them what to expect. This education reduces anxiety by putting the consumer in control to understand their health issues and presenting options to address them.
2. Evaluation
Shared Decision Making tools are ideally designed for “preference sensitive conditions” where there are multiple clinical options (For information about target conditions, see the recent report on the Dartmouth Atlas Project which was developed with The Foundation for Informed Medical Decision Making). The most effective tools offer alternatives, capture preferences and guide the consumer through the process while documenting their decisions. This helps set expectations for their experience and supports the discussion with their doctor or care coach.
3. Collaboration
As the patient and clinician/coach review the SDM summary document together, they can discuss questions, concerns and comments to make the best decision.
Health Plans Leverage Shared Decision Tools
During the panel, health plans described using Shared Decision Making tools to engage members in two key areas:
- Medical Home
Panelist Zev Lavon, PHD, Director Solution Architecture, CareFirst BCBS emphasized “the story of the patient is not their last doc visit or lab test”. CareFirst launched their Primary Care Medical Home initiative across a panel of physicians deploying communication tools to push information to patients to support the management of their chronic conditions.
-
Wellness Coaching
According to Mark L. Robitaille, MBA, Head of Care Management Support & Engagement, Aetna puts these tools into the hands of their health coaches to send emails with resources links to members or use the tools to look up information for the members without internet access.
Independent Health panelist, James J. Mis, MBA, Communications Manager, Health Care Services, described their interactive voice response campaign to inform members about viewing a shared decision making video (from Emmi Solutions) selected for their specific health interest.
Emerging Mobile SDM Tools
With a high penetration of smart phones and strong usage across minorities, health care organizations are realizing the tremendous opportunity to deploy mobile applications to engage consumers. To date, most health mobile health applications have been focused on wellness with educational information and tracking.
Panelist Changrong Ji, Senior Solutions Architect, CareFirst BCBS described the opportunity for mobile shared decision making tools. In the future, she envisions that sensors will capture the context of the consumer’s daily life, database analytics will identify patterns and machine learning will be used to help identify relevant mobile messages to send back to the consumer.
Healthwise’s View on Patient Response
During the Shared Decision Making Summit, the chairperson, Don Kemper, Healthwise’s CEO discussed the opportunity for shared decision making tools to give a “voice to the patient”. After the physician prescribes health information, the tool gathers patient’s preferences to document them in the medical record. I strongly agree with Don as he explains “there is no better way to engage the patient than to assure them that their voice will be heard in treatment and care plan decisions”.
Shared Decision Making Tools for Your Consumers
What are you doing to bring Shared Decision Making Tools to your consumers to motivate engagement in their health and wellness? I can help guide you through the process of identifing, evaluating and piloting these technologies to deliver better outcomes and a better experience for your consumers.