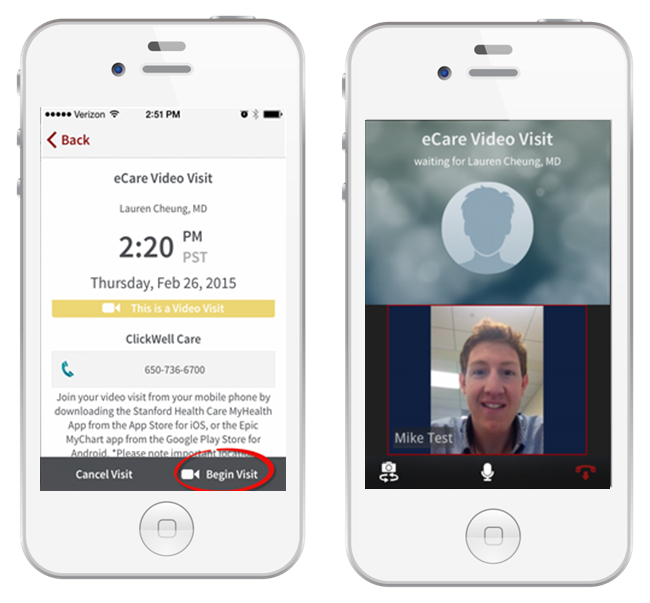
In January 2015, Stanford Medicine launched ClickWell Care, a new type of Primary Care clinic which leverages technology to allow patients to virtually connect with their own Stanford primary care clinicians and wellness coaches via video or phone visits. Patients use the MyHealth mobile app to schedule and conduct a video visit and share home health device data with the care team. Through this model, patients can choose to receive all of their primary care including integrated wellness coaching virtually, unless the physician indicates the need to come into the clinic for vaccinations, pap smears, procedures, or other physical exam needs.
In January 2015, Stanford Medicine launched ClickWell Care, a new type of Primary Care clinic which leverages technology to allow patients to virtually connect with their own Stanford primary care clinicians and wellness coaches via video or phone visits. Patients use the MyHealth mobile app to schedule and conduct a video visit and share home health device data with the care team. Through this model, patients can choose to receive all of their primary care including integrated wellness coaching virtually, unless the physician indicates the need to come into the clinic for vaccinations, pap smears, procedures, or other physical exam needs.
“Initially we created this virtual model for our ACO. We knew that 18-30 year olds were not interacting with primary care and were choosing to go to the Emergency Department or urgent care for their needs. During focus groups with this patient population, we learned they were so busy and didn’t have time to come into the office but really valued the relationship with their doctor. They wanted to receive care from their doctor but it wasn’t available in a way that was convenient to them. We knew that we needed to use technology to help support this relationship and not replace it”, explains Sumbul Desai, Medical Director ClickWell Care and Vice Chair of Strategy and Innovation in the Department of Medicine at Stanford University School of Medicine.
ClickWell clinicians and coaches support healthy patients and the ‘rising risk’ (e.g. up to 2 conditions), who are employees of Stanford University, Stanford Adult and Children’s Hospitals. With this highly educated, tech savvy patient population, there is a tremendous opportunity to leverage mobile tools to enhance the patient experience.
Patients see a doctor for primary care visits and engage with a wellness coach on health goals (i.e. weight loss, stress, activity, and nutrition) and to receive support for chronic conditions (i.e. diabetes, hypertension and hyperlipidemia). “The average age of a ClickWell patient is 36 years old. However, we have a growing group of 40-65 year olds, part of the ‘rising risk’ population, who prefer to do the majority of their visits virtually. These patients feel comfortable interacting by phone or video because they have a better understanding of the healthcare system and their health goals than our younger patients”, Desai shares.
The ClickWell Care program is designed to give patients complete control over how they want to access and interact with their doctor/coach and convenience of extended hours. Although patients have the option of scheduling a face to face appointment, they are incentivized to participate in a “no fee” virtual phone or video visit. Patients simply log into the MyHealth portal for their virtual appointment.
To date in the ClickWell program, there have been 2,142 visits; 43% conducted in-person, 32% through phone visits and 25% via video visits. ClickWell staff have seen 1,223 patients. Although 30% of new patients start off with a virtual visit, most prefer to meet their doctor first in-person. After an initial face to face visit, 60% opt to see their doctor virtually for their return visits via phone or video.
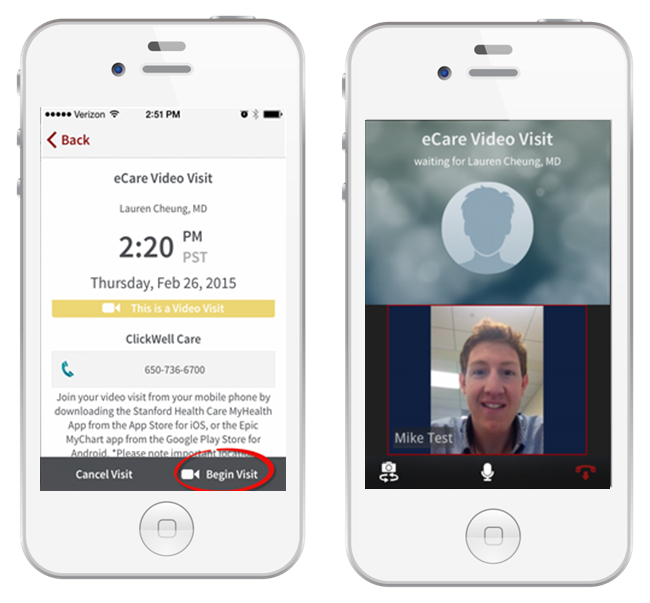 MyHealth Mobile AppAll patient information from the virtual visit is transmitted to the Epic EMR and is accessible through the MyHealth portal. Patients can ask follow up questions through the portal. When patients need to have blood work done, they are directed to the lab without having to come into the doctor’s office, and lab results are incorporated into the EMR with portal access. “Stanford was the first to use Epic’s integrated telemedicine service because we wanted this visit information available to patients in the portal and clinicians in their daily workflow”, confirms Lauren Cheung, Physician, ClickWell Care, and Medical Director, Strategic Innovations at Stanford University School of Medicine.
MyHealth Mobile AppAll patient information from the virtual visit is transmitted to the Epic EMR and is accessible through the MyHealth portal. Patients can ask follow up questions through the portal. When patients need to have blood work done, they are directed to the lab without having to come into the doctor’s office, and lab results are incorporated into the EMR with portal access. “Stanford was the first to use Epic’s integrated telemedicine service because we wanted this visit information available to patients in the portal and clinicians in their daily workflow”, confirms Lauren Cheung, Physician, ClickWell Care, and Medical Director, Strategic Innovations at Stanford University School of Medicine.
“One myth about telemedicine is that many patients choose to do video visits over phone visits. The truth is that it is an extra effort for the patient to participate in a video visit since the patient needs to be in front of a computer or mobile screen versus the phone visit which can be done while walking around”, Cheung adds.
“Back in 2013, we rolled out video visits as part of our primary care practice but we didn’t see a strong uptake. When we conceived the ClickWell Care program, we knew that we needed to introduce wellness coaching to provide a complete overall healthcare experience and deliver a higher level of healthcare service to our patients”, describes Desai.
Strong collaboration with IT and Operations have been pivotal in implementing this new care model. Through this collaboration, ClickWell has been able to leverage the new MyHealth app developed internally and has worked closely with IT to improve the platform and video visit capabilities to provide an excellent patient experience.
As part of the ClickWell Care program, the MyHealth mobile app helps strengthen care collaboration. The doctor/coach prescribes the health tracking app to the patient as a way to monitor key measures which may include steps, weight and blood pressure. The patient uses the MyHealth app to upload tracking data from Withings, Fitbit and Apple HealthKit to the EMR, sharing health status between visits. “When I see a patient with blood pressure trending higher, I ask the patient to schedule an online visit so that we can discuss how to address this through diet or medication changes”, Cheung explains.
ClickWell Lessons Learned
The Stanford Medicine team has gained insight into ClickWell Care program usage, the telehealth platform and mobile app to bring the most value to primary care patients and providers. They understand that it is not about the technology but instead about how the technology is put into the care model through a program.
Patients have shared many positive comments about the ClickWell Care program:
“Video visits allowed me to continue with pressing work concerns, instead of taking time off work to travel to a clinic. Video visits allowed me to chat with a Doctor late in the evening, and appointments were very easy to get. I felt that my virtual care was more personalized and provided a better experience.”
“I have not had many medical issues until recently. It is such a relief being able to ask questions and get answers quickly. My wellness appointments have me watching my diet and exercise regimen. Everything is done efficiently. I cannot say enough about the whole team that has been watching over me.”
“My experience with the ClickWell Clinic has been extremely informative and remarkably efficient. The flexibility they offer works perfect for people with busy schedules, without sacrificing the quality of care. The model of the Clinic makes other forms of healthcare communication feel outdated.”
“I have never had better communication and quicker responses than I have since becoming part of this program. I travel a lot and therefore keeping up via phone calls is not that practical. Being able to send messages electronically and to have an appointment via video chat is ideal.”
Doctors and wellness coaches have provided mostly positive feedback as well:
“Overall my experience with virtual visits in the clinic has been very positive. Compared to my previous experience with only in-person visits, it seems like the virtual option may make wellness patients more likely to continue with follow-ups. The integration with the doctors is also helpful in learning more about the patients and providing well-rounded care. It is a unique experience to be able to discuss treatments so closely with the patient’s doctors and in such a timely manner.”
“The integration of clinical care with wellness coaching has been phenomenal. I couldn’t imagine going back to health coaching without it. I am able to provide more targeted, individualized, and thorough care to my patients since I have full access to their medical records, provider notes, and work directly with their primary care physicians. Working directly alongside physicians has helped me to expand my knowledge on chronic disease management, stay up to date on clinical guidelines and recommendations.”
“As a provider, the technologies we use in this clinic allow us to quickly connect with our patients and address concerns for our patients proactively. The extended hours also allow for expanded patient access, as well as a flexible schedule for providers who staff the clinic who may desire alternative hours outside of the usual 9-5 business day.”
“Through our discussions with patients, we have also heard some suggestions for change. In the beginning, we were contacting patients to convince them to switch from in person to virtual visits. This frustrated some patients and most wanted to stay with the modality that they had initially chosen”, Desai shares.
Future ClickWell Care
As with other healthcare systems across the country, Stanford Medicine sees what is happening with the retail pharmacies increasing care access to patients. However, they believe this only fragments care because the visits are outside of the patient/doctor relationship. ClickWell Care is designed to be “longitudinal” and not episodic.
In 2016, Stanford Medicine is looking to extend into specialty care. “We are interested in integrating preventative cardiology for our patients since care entails discussing and improving risk factors for cardiovascular disease, which can be done virtually. Preventative cardiology patients would also benefit from wellness coaching to improve their risk factors for disease.
We also want to expand the use of connected health devices. Currently, very few patients upload and share their data with our care team. We are planning to incorporate this health tracking into a program for a patient population (e.g. specific chronic conditions) and integrate this information into clinical workflow to ensure that these patients receive excellent care. With our Precision Health initiative, we are not just interested in treating illness but rather finding tools to deliver a personalized health and wellness experience to ensure the best outcomes”, Desai concludes.
 Motivation for health and wellness,
Motivation for health and wellness,  educating consumers about health and wellness,
educating consumers about health and wellness,  online health and wellness coaching,
online health and wellness coaching,  patient education,
patient education,  patient experience,
patient experience,  patient journey,
patient journey,  personalization for health and wellness in
personalization for health and wellness in  AI consumer engagement,
AI consumer engagement,  Care collaboration,
Care collaboration,  Connected Health,
Connected Health,  Data Driven Health Engagement,
Data Driven Health Engagement,  Decision Support eHealth,
Decision Support eHealth,  Patient Decision Support,
Patient Decision Support,  Patient Engagement,
Patient Engagement,  Personalization eHealth,
Personalization eHealth,  patient health education
patient health education