Entries in educating consumers about health and wellness (50)
Providence Saint John uses AI platform to Empower Cancer Patients & Providers for Better Care
 July 20, 2023
July 20, 2023  In October 2022, Providence Saint John's Health Center invested in Project Ronin, an AI driven cancer intelligence platform to empower cancer patients and their clinical teams to manage treatment symptoms, care communications and clinical decision support. Their goal is to reduce ED visits and deliver better patient care and outcomes.
In October 2022, Providence Saint John's Health Center invested in Project Ronin, an AI driven cancer intelligence platform to empower cancer patients and their clinical teams to manage treatment symptoms, care communications and clinical decision support. Their goal is to reduce ED visits and deliver better patient care and outcomes.
According to the American Cancer Society’s 2023 Cancer Statistics report, cancer remains the second highest cause of death after heart disease. This is an estimated 2 million newly diagnosed cancer cases resulting in about 610,000 deaths.
Dr. Martin, MD, CMO of Providence Saint John’s believes that providing a new “space where cancer people can engage with their physicians has some very real, tangible benefits.” The digital tool is designed to support “patients with less-critical symptoms, which has the potential to reduce emergency department visits and improve clinical efficiency, which means a more efficient utilization of resources. Of course, we always advocate patients to come to the emergency department if they believe they are experiencing a medical emergency.”
Cancer Care Collaboration
Successful treatment of cancer is multifaceted, requires a multi-disciplinary care team, entails managing different data sets with continuous capture and monitoring of data, and has data complexity given the non-linear nature of the disease (i.e. diagnosis, treatment, remission, recurrence, treatment, survivorship/death).
Patients struggle to manage their cancer, both mentally and physically. Patient treatment symptoms can be severe. Questions come up between treatments but care teams are extremely busy. Patients need to remain connected to care teams to stay engaged, better manage, and communicate side effects.
Providers try to navigate their inefficient clinical workflows, address the administrative burden due to documentation requirements, and deal with workforce shortages. Today, providers spend 20-40 minutes finding patient info to prepare for patient visits, sometimes missing key data. Providers are overwhelmed to make needed decisions for cancer patients at the point of care.
AI Cancer Platform Delivers Care & Decision Support
The Ronin Cancer Platform enables patients to “take control of their care in a way that wasn't possible before and feel better connected to their care teams,” explains Dr. Neil Martin, MD, CMO of Providence Southern California Clinical Institutes and Executive Director of Saint John's Cancer Institute. Clinicians utilize this cancer intelligence platform’s predictive analytics and clinical dashboard to define treatment pathways and support more informed care decisions.
How does this work? The Ronin cancer platform takes structured and unstructured data from different EHR silos, and then cleans, calibrates, contextualizes this information to present care insights. With predictive analytics, providers can identify at-risk patients and see a complete real-time view of the care journey for immediate actions.
AI Data- Driven Cancer Platform: Patient Experience

Patient Patricia (patient persona), 74 years old, is newly diagnosed with breast cancer. While meeting with her new care team, Patricia learns about new resources including the free Ronin Symptom Monitoring App, to educate and support her as she navigates her cancer path. During her next appointment, Patricia notices the poster in her doctor’s office prompting her to download this patient app.
Patient Symptom Monitoring App Poster:
We want to support you through your treatment. In between your visits, please let us know how you're feeling by using the Ronin Symptom Monitoring Application. This will help us catch any side effects that you may experience. Studies show that symptom monitoring can ...
• Help people live longer and improve their quality of life
• Help people stay on treatment longer
• Lower visits to the emergency room and reduce hospital stay
Patricia downloads and begins using the Symptom Monitoring app which captures her Patient Reported Outcomes (PROs), enables her to track and manage side effects for treatment tolerance, displays her symptom history and provides her with personalized education based on what she is reporting. Within the app, Patricia selects from a list of symptoms and then sees a message that her symptoms “are concerning”, that her care team is monitoring this and will reach out to her within 24 hours.
AI Data-Driven Cancer Platform: Provider Experience

Patricia’s care team receives a “symptom alert” through the EHR based on the information that she has entered. Her symptom information has required a response (e.g. new symptom, moderate or severe symptom). The Nurse Navigator reaches out electronically or telephonically to check in on Patricia to understand more about her symptoms.
When her Oncologist Dr. Davis initially set up Patricia’s personalized care pathway on the platform, he indicated her specific disease type, which triggered patient reported outcomes surveys and at-risk surveys which captures data and intelligently prioritizes for the care team to take quick action to course correct and preempt adverse events.
While preparing for an upcoming office visit with Patricia, Dr. Davis uses the Ronin Platform to view a longitudinal timeline of her cancer journey, filled with real-time data (e.g. labs, images, pathology, treatment, surgery notes, past encounters) to make informed, proactive and personalized treatment decisions. Following the visit, Dr. Davis (or the clinical staff) pushes educational content to help Patricia to navigate her new symptoms or cancer stages.
AI Driven Care Experience Value Proposition
At Providence Saint John's Health Center, both patients and providers are finding value using the AI Ronin Platform, including clinical efficiencies, better care and outcomes and higher satisfaction. Here are some comments from the patient and provider users:
Patient Experience:
“Ronin provided confidence someone was monitoring me.”
“Ronin made me feel like my care team was with me, even at home.”
“I prefer not having to call the hospital. (With app) I am able to record side-effects right away as they are happening”.
“It’s (app) so easy to open up and write how I’m feeling…It’s a great reminder to me that even though I may think I’m fine, I need to pay attention to my symptoms.”
Provider/Staff Experience:
“We were able to catch an immune- related toxicity early for a patient of mine. Without Ronin, I would not have caught it”. Medical Oncologist
“We want to make sure the patients are having the best quality of life. With Ronin, we can check in on them more frequently.” Nurse Navigator
“From the treatment team’s standpoint, it’s made it easy to follow patients. It’s a great way to stay hands-on.” Nurse Navigator
“I had a patient straight up tell me ‘If it wasn’t for the app, I would be calling you guys every day'.” Medical Oncologist
“Visually, the Timeline tab makes it much easier to get up to speed on a patient. Especially compared to reading my colleague’s last notes.” Medical Oncologist
Success Metrics
In addition to gathering qualitative comments about the patient and provider/staff experience, Providence Saint John’s tracks quantitative success metrics for the AI driven Cancer Program. Some key metrics include:
● Reduced unnecessary ED admissions by >20% (early findings)
● Improved efficiencies with 35% decreased patient call volume and 32% patient-initiated messages.
● Strong patient satisfaction & experience
- 84% see positive impact on care experience
- 90% say app is easy to use
- 88% are satisfied with solution
Future for Providence with Ronin Cancer Platform
Moving beyond the patient mobile app and care communication from phase one, Providence Saint John's is planning to provide clinical decision support with oncology and risk dashboards and the capability to view comparative patient analytics in phase two.
"We are proud to implement evidence-based care solutions for patients in our community," said Brad Bott, Executive Director of the Southern California Clinical Institutes. "Our partnership with Ronin will help improve cancer care delivery while empowering our staff to practice more efficiently. It's a win-win."
Kaiser Permanente’s Reimagining Health Promotion & Behavior Change with Patients
 April 26, 2021
April 26, 2021  As one of the largest metabolic and bariatric surgery centers in the world, Kaiser Permanente Southern California sought to reimagine how it prepared and supported its patients every step of their journey. Kelly Dumke, DrPH, Senior Learning Consultant from Kaiser Permanente’s Center for Healthy Living presented their Human Centered Design process insights at MadPow’s Health Experience Design Conference HxD 2021 within the Person- Centered Care Experiences track.
As one of the largest metabolic and bariatric surgery centers in the world, Kaiser Permanente Southern California sought to reimagine how it prepared and supported its patients every step of their journey. Kelly Dumke, DrPH, Senior Learning Consultant from Kaiser Permanente’s Center for Healthy Living presented their Human Centered Design process insights at MadPow’s Health Experience Design Conference HxD 2021 within the Person- Centered Care Experiences track.Ochsner Health System’s O Bar & Digital Medicine Program Success & Expansion
 October 27, 2020
October 27, 2020  Ochsner Mobile O BarOver five years ago, Ochsner Health launched their O Bar (Apple genius-like concept) to support patients getting started with digital health tools. Today, Ochsner has nine physical O Bars located in the bottom floor of their health centers and one mobile O Bar.
Ochsner Mobile O BarOver five years ago, Ochsner Health launched their O Bar (Apple genius-like concept) to support patients getting started with digital health tools. Today, Ochsner has nine physical O Bars located in the bottom floor of their health centers and one mobile O Bar.
Although any Ochsner patient can visit the O Bar to begin using a curated set of digital health apps and devices, patients who are invited to join a digital medicine program can go to the O Bar to get set up with selected digital tools to manage and monitor their health journey. Digital medicine program participants have the option to have their digital tools sent via the mail, without going to the O Bar and can call their program tech support for any assistance. Pre-Covid, about 5-10% of patients chose to receive their digital health tools by mail. During the pandemic, it is mostly all mail.
 Ochsner Hypertension Digital Medicine ProgramTo date, Ochsner Health is offering digital management initiatives for hypertension, diabetes, pregnancy and the latest COPD program. Patients do not need to have access to WIFI to participate, just a smartphone or tablet. Less than 5% of patients participating in the digital medicine program use the tablet and instead have their apps downloaded to their smart phone.
Ochsner Hypertension Digital Medicine ProgramTo date, Ochsner Health is offering digital management initiatives for hypertension, diabetes, pregnancy and the latest COPD program. Patients do not need to have access to WIFI to participate, just a smartphone or tablet. Less than 5% of patients participating in the digital medicine program use the tablet and instead have their apps downloaded to their smart phone.
“Our digital medicine programs are realizing 2-3x better outcomes rates than the standard of care”, explains Dr. Richard Milani, Chief clinical transformation officer and innovationOchsner Medical Director, Ochsner Health. “In order to understand how these programs were designed, it is important to take a step back and think about how we need to help patients manage their chronic condition(s). First, we need more frequent data to know at any point in time if their chronic disease is under control. Second we must make sure individuals are prescribed guideline-directed pharmacotherapy. With the number of new medications coming onto the market and medical research about the profile of patients experiencing the best outcomes, we must be sure patients are having the best chance to achieve an optimal outcome. Finally, we need engage our patients on the “right behaviors” (e.g. nutrition, fitness, stress reduction).”
"We set up our digital medicine programs to be supported by a dedicated team who interacts with and manages the patient’s condition(s)”, shares Dr. Milani. “Their doctor invites the patient to join the program, but it is a digital medicine team who responds to the incoming data and alerts from the digital health tools.” Ochsner’s digital medicine team consists of a pharmacist/APP to help the patient with the “right guideline-directed medicine” and a health coach to provide guidance on lifestyle decisions using behavioral health science techniques. Patients that are on two of Ochsner’s digital medicine programs engage with the same pharmacist/APP and health coach, creating a holistic approach to patient care.
Patients access all of digital health tools in the digital medicine program area with their patient portal. A patient logs in to access patient education information (videos), communicate with her team by scheduling a phone call or sending asynchronous messages and view monthly reports which shows how she is doing, and progress made over time. The patient can also contact the digital medicine team for technical support for their digital tools, which is rare because these connected devices are easy to use for even less tech savvy patients.
 Ochsner Connected Mom Pregnancy Digital Medicine ProgramIn addition to appropriate connected devices given to patients to capture and transmit key measures (e.g. diabetes/wireless glucometer, hypertension/ wireless blood pressure cuff, COPD/wireless inhaler and pregnancy/ wireless blood pressure cuff & wireless scale), patients receive texts to capture changes in condition (e.g. COPD severity level), track self- efficacy measures or to be notified of a health concern (e.g. warning about the poor air quality level). Patients have the option of connecting in and sending more information such as weight measures from their own digital scale or steps from their fitness tracker to share with the digital medicine team.
Ochsner Connected Mom Pregnancy Digital Medicine ProgramIn addition to appropriate connected devices given to patients to capture and transmit key measures (e.g. diabetes/wireless glucometer, hypertension/ wireless blood pressure cuff, COPD/wireless inhaler and pregnancy/ wireless blood pressure cuff & wireless scale), patients receive texts to capture changes in condition (e.g. COPD severity level), track self- efficacy measures or to be notified of a health concern (e.g. warning about the poor air quality level). Patients have the option of connecting in and sending more information such as weight measures from their own digital scale or steps from their fitness tracker to share with the digital medicine team.
Program Success Measures & Expansion Plans
Ochsner has enrolled more than 15,000 patients across their digital medicine programs.
Over the past 5 years, Ochsner has received positive feedback from their digital management team (e.g. Pharmacist, Health Coach) and from patients in the program.
“The role of a clinical pharmacist isn’t always to add more medicine. We work with each person to incorporate lifestyle changes and medications that are right for them. This includes stopping or decreasing medicine doses when lifestyle changes lead to improved health.” -- Carrie, Clinical Pharmacist
“I work with individuals to make small, achievable goals that will not only improve their health, but ultimately improve the way they feel mentally and physically. This allows the patient to feel confident in themselves to make healthier choices in any situation.” – Christina, Professional Health Coach
“I like that it is private. I don’t have to take a blood pressure reading at a Walgreens or CVS. It’s encouraging to know that the lifestyle choices I’m making as well as my compliance to my drug regiment is having a positive effect.” – Alan, Digital Medicine Hypertension Program
“For anyone who has doubts about joining the program, I would say step out and take the journey.” – Lance, Digital Medicine Diabetes Program
“You get a lot out of Ochsner Digital Medicine. You get a family who is by your side every step of the way.” - Gaylan, Digital Medicine Hypertension Program
In addition to patient and staff feedback, Ochsner uses a set of quantitative measures to evaluate success. Dr. Milani is proud to share the Net Promoter Score of patients in the digital medicine program of 87.5, which indicates a high level of recommending the program to others.
Dr. Milani explains, “the key success measure is the reengineering of chronic disease care into a new model of care delivery. Our metrics of success are control measures for the disease (i.e. better blood pressure control, better diabetes control, etc.).”
Ochsner has plans to grow their digital medicine programs in 2021. “We are expanding the population we currently serve and will be adding more disease categories (like lipid management and others). We look at the prevalence of disease burden and the opportunities for better control when deciding on new digital medicine programs,” Dr Milani concludes.
 Permalink
Permalink  chronic care management,
chronic care management,  educating consumers about health and wellness,
educating consumers about health and wellness,  health coaching,
health coaching,  mobile health application,
mobile health application,  patient generated health data in
patient generated health data in  Connected Health,
Connected Health,  Data Driven Health Engagement,
Data Driven Health Engagement,  Mobile Health,
Mobile Health,  Patient Decision Support,
Patient Decision Support,  Patient Engagement,
Patient Engagement,  Patient Experience,
Patient Experience,  Patient Journey,
Patient Journey,  TeleHealth,
TeleHealth,  TeleMedicine,
TeleMedicine,  digital health,
digital health,  patient health education
patient health education Providence Health’s Bot Grace engages and guides patients to the digital front door for care
 February 25, 2020
February 25, 2020  According to the 2019 Accenture Digital Health Consumer Survey, patient’s expectations are increasing for providers to offer digital capabilities. Patients value convenience (appointment times, location) and are increasingly considering “non-traditional” service channels such as retail clinics and virtual care.
According to the 2019 Accenture Digital Health Consumer Survey, patient’s expectations are increasing for providers to offer digital capabilities. Patients value convenience (appointment times, location) and are increasingly considering “non-traditional” service channels such as retail clinics and virtual care.
Providence Health’s Innovation team continuously monitors these trends to identify ways to deliver a better patient care experience. “With the tremendous growth of chatbots and voice assistants, we decided to develop a virtual health assistant and begin to understand how to support the patients in their search for care”, explains Maryam Gholami, Chief Product Officer at Digital Innovations, Providence Health.
In fall 2018, Washington State based Providence St Joseph started developing and testing Grace, a chatbot which asks the patient about their symptoms and based on their location, time of the day and scope of services provided in various care options (virtual, clinics, or At Home) directs them to the best care. Eventually Grace was enhanced to also address frequently asked questions by patients.
Since the healthcare system is complex for consumers to navigate, Providence Health designed their digital tool to provide answers and guidance to help the patient find the right care and make the best care decisions. For example, a consumer may not know which modality of care to use (e.g. Emergency Room. Urgent Care, Retail Clinic, Virtual/Telehealth) or what symptoms trigger an immediate visit.
On the consumer side, Providence Health wants to stay aligned with their patient’s increasing expectations for service on demand. Consumers are already using digital assistants for shopping, banking and travel 24x7.
“From a business perspective, we want to provide accessible, convenient and affordable care. Therefore, we need to improve operational efficiency, free-up professional caregiver capacity for the right care and tasks, while increasing the care options and quality for consumers. We want to have our virtual health assistant take on the administrative tasks so that our clinical staff can focus on patient care. For example, Grace conducts a virtual patient intake to schedule a visit, collecting information such as reason for the visit, demographics, insurance and payment details”, explains Maryam. “This digital health assistant also assesses the best modality of care based on patient’s input and availability of care, matching the right resource to meet each patient’s needs. With this type of service navigation, Providence Health can ensure that the required license level is designated for the visit, reducing care cost and ensuring availability of providers for the appropriate level of care. Healthcare is supply-constrained, so this is a very important value.”
Patient Experience with Grace Bot
Providence Health has worked closely with the patients to design the Grace bot. Here is a look into the patient experience.
Patient Patricia who lives in Washington State, types her symptoms into Google to figure out what she has and where she can get care. Within her search results, Patricia sees a Providence Health website link and then meets Grace, a pop- up text chatbot ready to help her.
The Grace bot helps Patricia in two important ways:

1. Care Navigation: Given that Patricia needs “same day care” and has a low acuity health problem, she types into the Grace bot that she has a fever and sees that Grace has recommended a virtual visit or a same day clinic appointment. Patricia provides her zip code, chooses the clinic near her house and schedules an appointment for 7 PM that evening.
2. Customer Service/Concierge: Patricia has questions about whether her insurance is accepted and types in “what insurance do you take?” Grace provides a list of insurance options. Patricia can also ask for information to read about her health problem before her visit.
Patient Experience with Grace Bot
The Grace bot was designed for patients by patients. Throughout the development process, the product team at Providence Health worked closely with patients to understand the “tasks they were trying to complete” and defined how Grace needed to guide them through these steps. During testing, the team monitored where patients dropped off and tuned the messages to “optimize” their care journey.
“We are digging into the questions that our customers ask so that we can improve our knowledge base. This enables Grace to better respond to our patient questions”, Maryam explains.
With ongoing patient feedback, Providence Health has identified and has been addressing several areas to improve the patient experience.
Chatbot Persona: Maryam shares that “we used emojis to make the digital interaction more casual and friendly. Our patients did not like the emojis because they felt emojis do not convey trust which is essential when communicating health information. Patients also needed to feel comfortable that the responses and recommendations were not coming from a human. We are working on the right persona for Grace and defining the best interaction”.
Chatbot Behavior: Providence Health’s product team is determining when Grace needs to confirm information with the patient so that it accurately reflects her needs. There is a fine line between repeating back to be sure and being annoying to the patient who is looking to quickly complete her task (e.g. set up a visit). However, there is a risk of sending the patient to a modality that does not meet her needs (i.e. she needs to see a doctor and not an RN). “We need to understand the clinical operations from end to end so that we can define the business rules to successfully guide the patient interaction”, Maryam comments.
Consumer Adoption: Some patients are pleasantly surprised about what the Grace chatbot can do for them. Others may not understand what to ask her. Health organizations will need to educate consumers on the types of questions to ask so that patients can gain the most value when engaging with the bot.
Provider Adoption: Providence Health is working on enabling the Grace bot to support virtual care. Grace can engage with the patient to capture information prior to the telehealth visit. However, we need to ensure that this is designed and implemented in such a way that clinicians can properly review all of the information captured before the visit begins and that we are not increasing provider burn-out. It needs to improve the experience for both patients and providers.
Patient Representative Experience: When the Grace bot “hands off” the patient for the scheduled visit or for further follow up, it is important that the representative knows that patient just engaged with the Grace chatbot, has the context and the information already collected and can address the patient accordingly.
Chatbot Success Evaluation
Maryam shares some key success measures for the Grace bot. “We currently know that over 42% of our patients who engage with Grace get answers to their questions or get help navigating to the right modality of care. 18% of these engagements result in completion of appointments booked with one of our ExpressCare Clinics (Urgent Care). We are also learning which questions Grace doesn’t know how to answer or which tasks she can’t currently complete. This learning is very important to help us with our future product direction and iterations”.
Patients interacting with Grace can navigate to Providence Health’s ExpressCare options based on a chief complaint or use a symptom checker before choosing recommended ExpressCare options. Providence Health is seeing a 90% accuracy rate for patients that have been directed to ExpressCare from the patient’s chief complaint.
According to Maryam, there are weekly meetings with the product analytics team to understand how patients are using Grace so that they can enhance the patient experience. “We measure every interaction in the funnel to understand if we’ve helped users complete their tasks. Some of these measure include # of click rates, # of patients questions answered, # of appointments booked, # of visits completed along with type of visits, and chatbot engagement when the customer support center is closed”, describes Maryam.
 At the end of each interaction, Grace asks the patient if he is satisfied with the task – “Was I able to address your needs today”? According to Maryam, about 40% indicate that the Grace bot met their needs. Providence Health is closely listening to patient feedback to increase the satisfaction percentage.
At the end of each interaction, Grace asks the patient if he is satisfied with the task – “Was I able to address your needs today”? According to Maryam, about 40% indicate that the Grace bot met their needs. Providence Health is closely listening to patient feedback to increase the satisfaction percentage.
Providence Health has received insightful patient feedback about the Grace bot experience:
“This was the first time I’ve seen something like that, I thought it was extremely helpful. It asked a lot of good questions to get me the right help.”
“I felt like it was really easy to get an appointment. Very quick automated responses got me to the right place.”
“I thought it was excellent. I research a lot of my own health issues, so I’m excited about this. Anything that can help me learn about my symptoms and what to do about them, I’m excited for it.”
“For me, it was kind of cold. If it could change the wording to make it more human it would be better. I’d prefer a more human touch to it. I think in this field personality is important, so work on making it more warm, caring, and friendly.”
Future Plans with Grace:
Providence Health is committed to enhance the Grace virtual health assistant experience for patients by:
Expanding the patient journey: Currently, Grace is available more in the discovery phase, when patients are searching for care options. “Next, we are incorporating Grace into the Virtual waiting room to gather intake information before the patient participates in the telehealth visit. Our goal is to have Grace available when/where appropriate to help consumers navigation through health journey”, Maryam adds. “We are looking to move beyond low acuity to helping patients find and book PCP and Specialty appointments”.
Increasing the personalization: While Grace currently does some personalization based on consumer’s location, time and symptoms. Providence Health believes there is still a great deal of opportunity to leverage various sources of data including patient records. They will proceed carefully given the consumers’ data security and privacy needs.
Improving the High Tech & High Touch Collaboration: “We view our virtual assistant as an augmentation tool for our professional caregivers. We are working on creating a warm hand off to human caregivers with the conversation context. We are designing these tools so that based on consumer’s choice, human caregivers can step in to assist our patients”, explains Maryam.
Providence Health’s clinical and business leaders believe that offering these virtual health assistants are essential to delivering the best care experience for the patient, today and in the future.
“We are levering technology to connect the consumers to the right place for care with the right service and providers at the right time. AI is going to help us to improve the seamless experience.” Thanh Nguyen, Executive Director and Chief Clinical Officer of Express Care
“AI-powered virtual assistants will have a significant impact on healthcare by engaging consumers through voice/chat, a more natural way of interaction, and by intelligently automating mundane tasks and simplifying complex ones at scale.” Aaron Martin, EVP, Chief Digital Officer
 Permalink
Permalink  chatbot,
chatbot,  consumer generated health and wellness content,
consumer generated health and wellness content,  educating consumers about health and wellness in
educating consumers about health and wellness in  AI,
AI,  Care access,
Care access,  Care collaboration,
Care collaboration,  Connected Health,
Connected Health,  Data Driven Health Engagement,
Data Driven Health Engagement,  Decision support,
Decision support,  Mobile Health,
Mobile Health,  Patient Decision Support,
Patient Decision Support,  Patient Engagement,
Patient Engagement,  Patient Experience,
Patient Experience,  Patient Journey,
Patient Journey,  TeleHealth,
TeleHealth,  Virtual Health Assistant,
Virtual Health Assistant,  digital health,
digital health,  patient health education
patient health education Northwell Health’s Patients engage with AI ChatBot for guidance & support through their care journey
 November 6, 2018
November 6, 2018 Northwell Health, New York’s large integrated health system with 22 hospitals and 550+ outpatient facilities, recognizes the importance of leveraging technology to extend the care team and personalize the patient journey.
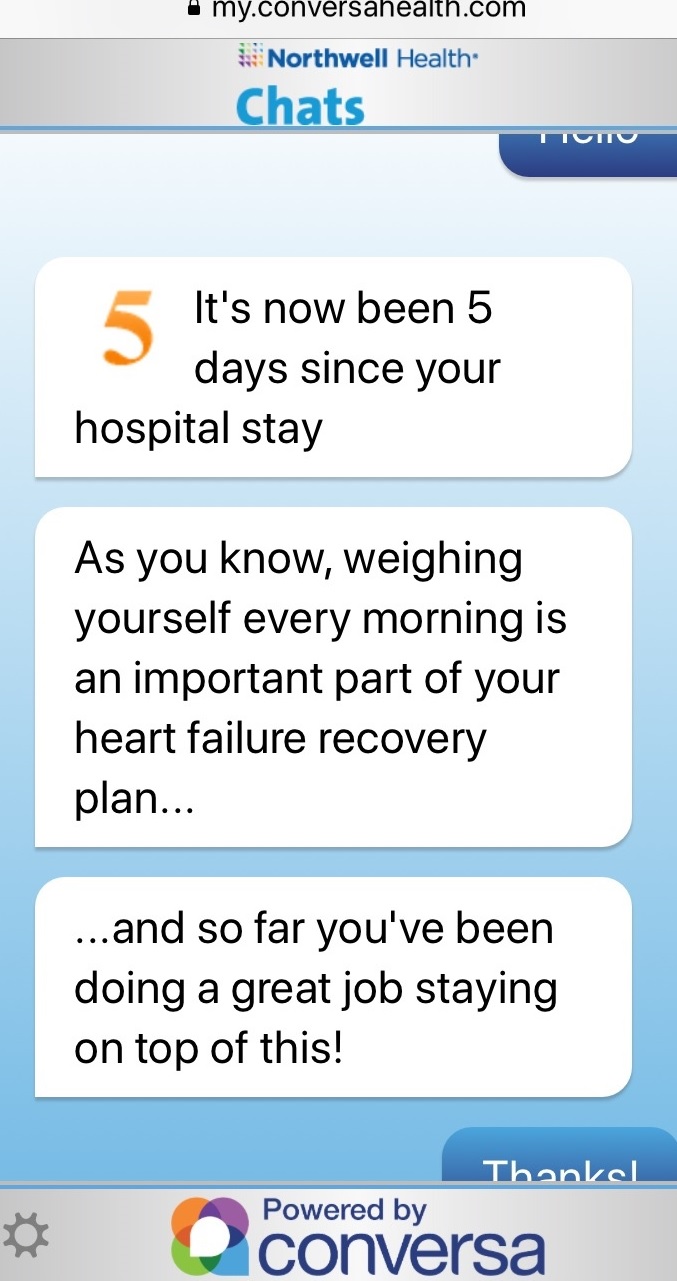
With the launch Northwell Health Chats (powered by Conversa Health), patients are empowered to connect, communicate and collaborate with their care team, while their clinicians closely monitor the patient’s evolving needs.
 Think about a patient’s journey today. Pamela, a 78 year old Medicare patient has just been discharged from a Northwell Hospital for a heart failure episode.
Think about a patient’s journey today. Pamela, a 78 year old Medicare patient has just been discharged from a Northwell Hospital for a heart failure episode.
Fortunately for Pamela, Northwell’s Health Chats, a new conversational AI platform will help support her during her recovery. With this text based chatbot, Pamela receives many more outreaches from her care team, a three- fold increase from about five times to fifteen during the 30 days post discharge period.
When she returns home, Pamela starts receiving notifications through SMS text message and clicks on the link to begin her chat about how she is doing. These chats continue to support Pamela through her recovery.
Pamela is asked to confirm her weight uploaded automatically from her Withings scale. She sees her weight trending map with an educational message about working towards her goal. Next, Pamela responds how she is doing with her leg swelling and then about any difficulty breathing.
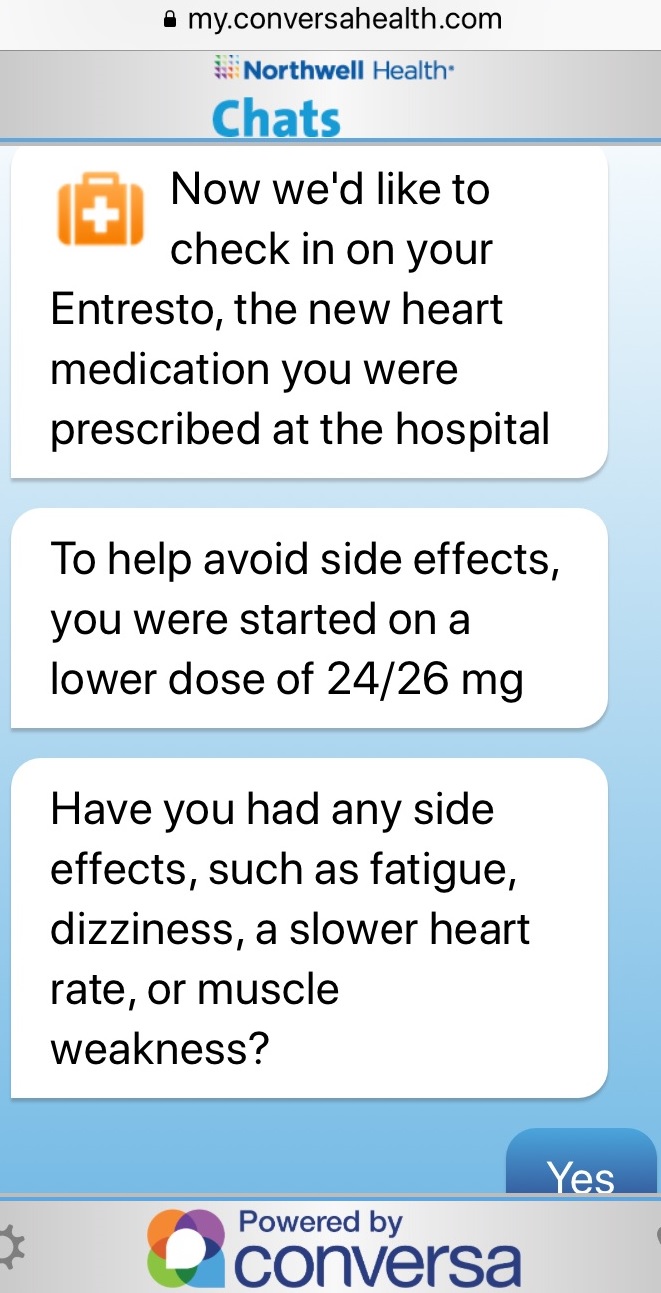 Finally, the chat asks Pamela to indicate any side effects of her new medication. Based on her responses, she may be connected with her nurse to discuss any medication adjustments. All of the information that Pamela provided to the chatbot is shared with her nurse for their discussion.
Finally, the chat asks Pamela to indicate any side effects of her new medication. Based on her responses, she may be connected with her nurse to discuss any medication adjustments. All of the information that Pamela provided to the chatbot is shared with her nurse for their discussion.
Since this patient engagement solution is seamlessly integrated into Northwell’s work flow (e.g. care management tool/HIE), Pamela receives these personalized chats from her specific Nurse Navigator at Northwell and the chat content is tailored for her specific care journey. Pamela trusts the information that she receives and can respond with questions and concerns at any time. Pamela’s Nurse Navigator will determine if she needs to come right in to the office or if they can address her issues through a text, email, call or telehealth visit.
Northwell is leveraging their Health Chats for population health. For example, the chat support patients as they prepare for a colonoscopy in their own language, ensuring the patient understands the instructions and knows how important this screening is to their health. This chat helps increase the patient’s health literacy and confirms that the patient knows how to prepare, reducing delays in diagnosis and additional health costs.
Positive Results with Northwell Health Chats
Sabina Zak, VP Northwell Community Health believes this chatbot is a “way to engage patients, by embedding information that is accurate, actionable and enables them to make more informed decisions which leads to better outcomes”.
As Northwell rolls out their Health Chats across the enterprise, they will be monitoring care quality, care cost and patient satisfaction measures. With Northwell Health Chats, they are seeing a 97% patient satisfaction rate and lower post-acute care expenses in some of its hospitals. Northwell management is particularity interested in the reduced costs from fewer outreach calls since the bot engages patients and brings back needed information.
Patient Comment:
“These conversations were great and supportive emotionally as well as medically”.
Nurse Leader Comment:
“Conversa gives me reassurance that my patients are ok because I can see that they are responding to the health chats. It gives me piece of mind knowing that they are alright without having to always call them.”
Clinical Leader Comment:
“Innovative technologies like Northwell Health Chats are critical assets in our journey towards providing excellent clinical care and an outstanding personalized patient experience”, explains Northwell Health physician Dr. Zenobia Brown, VP Population Health.
Expanding Conversational Chat at Northwell Health
In addition to supporting patients through procedures such as Colonoscopies, Northwell will be using this conversational chatbot to gather social determinants of health before the patient’s annual office visit. This information will be shared with their care team for their appointment.
Beyond population health, Northwell is expanding their Health Chats into Oncology, starting with head and neck and expanding to breast and prostate cancer patients. Northwell’s Health Chats will help patients prepare for the treatment, manage symptoms and check in once the treatment has concluded.
In the future, Northwell is planning to use their Health Chats in the areas of bundled payments for patients with Coronary Artery bypass, Acute MI, Pneumonia, Stroke and Heart Failure.
“Conversa’s conversational AI powering Northwell Health Chats enables us to improve care coordination, patient satisfaction and our ongoing patient relationship, resulting in the improved well-being of our customers while reducing costs. This high-tech, high touch, scalable approach benefits our patients, our nurses and our health system”, concludes Joseph Schulman, SVP Regional Executive Director at Northwell Health.
 Motivation for health and wellness,
Motivation for health and wellness,  educating consumers about health and wellness,
educating consumers about health and wellness,  online health and wellness coaching,
online health and wellness coaching,  patient education,
patient education,  patient experience,
patient experience,  patient journey,
patient journey,  personalization for health and wellness in
personalization for health and wellness in  AI consumer engagement,
AI consumer engagement,  Care collaboration,
Care collaboration,  Connected Health,
Connected Health,  Data Driven Health Engagement,
Data Driven Health Engagement,  Decision Support eHealth,
Decision Support eHealth,  Patient Decision Support,
Patient Decision Support,  Patient Engagement,
Patient Engagement,  Personalization eHealth,
Personalization eHealth,  patient health education
patient health education