 ManyStrong Social Community SupportAs soon as he walked through the door at Starbucks, I knew something was terribly wrong. I have known Ben for more than ten years and he has never looked like this. Ben appeared extremely exhausted, had lost his smile and gained a few pounds since our last tea together.
ManyStrong Social Community SupportAs soon as he walked through the door at Starbucks, I knew something was terribly wrong. I have known Ben for more than ten years and he has never looked like this. Ben appeared extremely exhausted, had lost his smile and gained a few pounds since our last tea together.
After he dropped his keys on the small round table and sat down next to me, I asked Ben what was happening. His elderly mother had fallen again in her bathroom. Ben had been shlepping her from the hospital to her apartment, running to the pharmacy to change her medication for the third time this week and food shopping to make sure she had what she needed. As I listened to Ben, I wondered how his brother Rob or other family members were helping out. Just because Ben is the oldest child doesn’t mean that he needs to take on all of the responsibility. Caring for his mother day in and day out was taking a toll on my friend’s health.
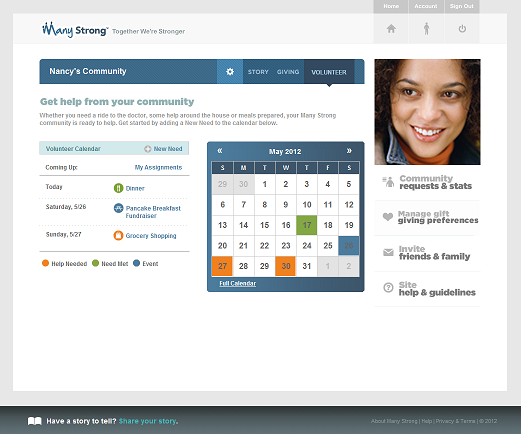
When he stopped talking to take a breath, I started telling Ben about ManyStrong, the new social community initiative from UnitedHealth Group. ManyStrong is a free new social tool that Ben can use to create an online community to support his mother, Evelyn. When friends and family ask “how can help”, Ben can invite them to Evelyn’s private community which has tools for them to contribute in some way.
Over the past few years, I have worked with many different social communities but this one is different:
Personalized Social Community On Demand: Ben can create a community for the specific purpose of supporting his mother. Within the community, Ben can provide updates and request the help that he truly needs to care for his mother. Knowing Ben, it is easier for him to ask for help this way than it is to pick up the phone to call those who had offered help in the past.
Action Driven Support: By following the link in Ben’s email invitation, friends and family can provide support in their own way. After all, some are a few miles away and others are across the country.
- Financial Support: They can donate money which will be placed on a cash card or purchase a gift card for Evelyn.
- Motivational Support: Her loved ones can leave care messaging to encourage Evelyn on a daily basis, motivating her to get stronger.
- Story Telling For Support: Ben and others in Evelyn’s community can upload pictures and videos to share. Seeing a photo of Evelyn walking after her fall may bring relief to her loved ones. Ben can enter comments that “mom has her dancing shoes ready” which may bring a smile to their faces, easing their anxiety for a moment.
- Physical Support: When Ben adds new requests for help within the ManyStrong community, friends and family can take on the responsibility to make a meal, run an errand to the store, spend time with Evelyn or simply check- in on her. The calendaring feature automatically tracks the need and the person taking on that need for all to see in the community.
ManyStrong Back Story
“We created ManyStrong simply to help people more easily help each other. When people we know get sick, or go through a sudden medical emergency or other serious health event, we naturally want to help them. They are our friends, our families, people we care about. It’s tough to know how to help. And with everything that person is dealing with, it’s hard to find out what you can do to help without putting additional stress on them and their family. That’s where ManyStrong comes in”, explains Kunjorn Chambundabongse (KC), VP Innovation and R&D, UnitedHealth Group.
When serious health issues arise, people turn to online communities for support. Many communities are designed for the individual with the health problem but not necessarily to support the caregiver. In their February 2011 Peer- to -Peer Healthcare research, Pew found 59% turn to family, friends and fellow patients when needing “emotional support in dealing with a health issue”.
How is UnitedHealth providing a unique social community solution? KC clarifies ManyStrong’s differentiation. “Yes there are many communities out there doing pieces of this. Some sites focus on the medical and clinical related side, allowing people to connect with others going through similar illnesses and share treatment data. Other sites focus on the non-clinical side, such as fundraising or keeping people informed through journaling/blogging. And you have many people using the big sites like Facebook, but privacy and security are huge problems with something as serious as health. ManyStrong brings all these tools into one place in a private and secure way, and allows the caregiver community manager to create a safe spot for people to rally together to support a person or family they care about.”
The ManyStrong social community solution can be used to support many different situations such as for a child with the long term illness, a senior aging at home or a co-worker battling a disease. Sometimes companies cannot envision the use cases before launching their offering into the marketplace. KC has thought about the various situations and shares ”we don’t know exactly how people will use Many Strong but we make it our mission to learn from them. When we look at users or potential users of Many Strong, we ask if there is any way that we can make the product better for that family, that community, for the people they’re supporting based on how they’re using it. One community could have hundreds or even thousands of supporters, or it could have a handful of very close supporters.”
What does success look like? KC explains “success to us is about celebrating the actions of people helping one another. Millions of messages of encouragement, millions in donations to families, and millions of hours of volunteered time… so many beautiful and meaningful actions. Success to us is seeing all these actions across our country and across the world, one community at a time.”
During their initial beta phase, UnitedHealth is offering the entire community site for free and is even covering the transaction fee on the donated money. KC describes their evolving business model for the ManyStrong Community. “Eventually we will need to charge small fees to cover bank transaction processing costs. We are also exploring integration with other service providers such as meal delivery, professional in-home care, and other features to provide even more options for people to give. We may earn referral fees from these merchant partners over time. While the site may earn some revenue, our mission is to give back profits to charitable organizations that will further benefit users of ManyStrong.”
Note: December 2013, UnitedHealth discontinued their ManyStrong website.
 educating consumers about health and wellness,
educating consumers about health and wellness,  family ehealth engagement,
family ehealth engagement,  online health and wellness support,
online health and wellness support,  patient education,
patient education,  patient ehealth engagement in
patient ehealth engagement in  Behavior Change Health & Wellness,
Behavior Change Health & Wellness,  Data Driven Health Engagement,
Data Driven Health Engagement,  Decision Support eHealth,
Decision Support eHealth,  Employee Engagement Health & Wellness,
Employee Engagement Health & Wellness,  Patient Centered Medical Home,
Patient Centered Medical Home,  Patient Decision Support,
Patient Decision Support,  Patient Engagement,
Patient Engagement,  shared decision making ehealth
shared decision making ehealth