Permalink
Permalink Entries in Online consumer/patient advisory board (6)
UCSF's Comprehensive Co-Design Approach for Pediatric Patients growing up with Chronic Illness
 April 27, 2021
April 27, 2021  The journey for pediatric patients with multiple co-morbidities can be complex, with some patients receiving care from 20+ providers. Jan Yeager, Service Designer, UCSF shared experiences co-designing a Chronic Illness Center with patients, caregivers, UCSF physicians and clinicians, and community providers at MadPow’s 2021 Health Experience Design Conference.
The journey for pediatric patients with multiple co-morbidities can be complex, with some patients receiving care from 20+ providers. Jan Yeager, Service Designer, UCSF shared experiences co-designing a Chronic Illness Center with patients, caregivers, UCSF physicians and clinicians, and community providers at MadPow’s 2021 Health Experience Design Conference.Deja Vu. Data- Driven Retail Strategies, For Health Care This Time
 April 9, 2012
April 9, 2012 
Health care companies today are following in the footsteps of the retail-oriented, information based financial services industry.
What financial services companies have discovered is that in order to build their business, they must build a personal relationship with the consumer. They accomplished this by creating a consumer-centric database, monitoring shopping behavior through reporting and analytics, motivating activity through multi-channel communications and launching a loyalty program to reward consumer spending,
I was part of this customer-centric transformation as the Director of Database Marketing at GE Capital, which provides private label credit card programs for Disney and Apple, to name a few marquee brands. My cross- functional team started with the consumer in mind. We envisioned the experience that our retailer customers needed to deliver to their consumer card holders to differentiate themselves in the marketplace and capture a larger mind share and business share.
This is the same path that health care companies are marching down to get ready for new customers.
Consumers Are Coming! Health Care Companies Invest in Retail Strategies
In their report on “The Era of the Health care Consumer,” Accenture describes the shift in responsibility from the employers to the consumers and the resulting health care company investment changes from BTB to BTC. Accenture cites the opportunity to learn from the retail sector, especially the segmentation, profiling, loyalty and cross channel communications.
A few health care organizations are making the needed investments to move closer to the consumer in order to better understand their needs for information and tools to support health management. Aetna, for example, has partnered with Best Buy to sell wellness programs to consumers within the retail store and deliver their wellness coaching program online. In addition to store fronts, Florida Blue (previously BCBS Florida) has invested in their Guidewell online initiative to build a relationship with consumers beyond their member base.
Most health care companies, however, are still trying to figure out where to begin.
Barriers for Data-Driven Retail Health Care
There are several key barriers that Health care companies must overcome in order to effectively engage these retail consumers.
- Knowledge about the New Consumer: Health care companies have limited or no information about their newest customer that is either considering their health product/service or has just come onboard. As a result, the interaction can feel less satisfying. Using best practices from the financial industry, health care organizations can utilize segmentation and profiling to deliver a more personalized experience while gathering knowledge about the consumer through each touch.
- Knowledge about Consumers' Data Needs: During their recent research, IDC Health Insights learned that “despite large investments meant to extend the organizations’ consumer-centric model, health plans know little about how consumers want to consume information…”. Financial Services companies remain aligned with their customers by inviting them to participate in their own private branded online research community. The company captures consumer input and feedback on their product road map and new marketing initiatives.
- Knowledge about Proactive & Personalized Communications: Many health care organizations wait for consumers to come to their online marketing destinations including their website and social media and then wait for them to return. Although these companies maybe have tools in place to capture the contact information of interested consumers, they tend to send out the same information to everyone. Financial Services companies segment these target consumers and stream content of interest across their preferred communication channels to bring them back and engage.
- Knowledge about Developing a Personalized Incentive Program: One way that health care companies can differentiate themselves is with an incentive program that rewards a consumer for healthy lifestyle behaviors that fit her profile. One of the reasons that some credit card loyalty programs (e.g. American Express) are so effective is that they target personalized offers based on each consumer’s spending behavior profile.
Health care companies can learn from the leaders in the Financial Services industry about how to leverage technology to build a retail consumer relationship through ongoing personalized communications and programs which are aligned with the consumer’s ongoing data needs.
Regence Reaches Step 3 on their Consumer Engagement Path
 February 14, 2012
February 14, 2012 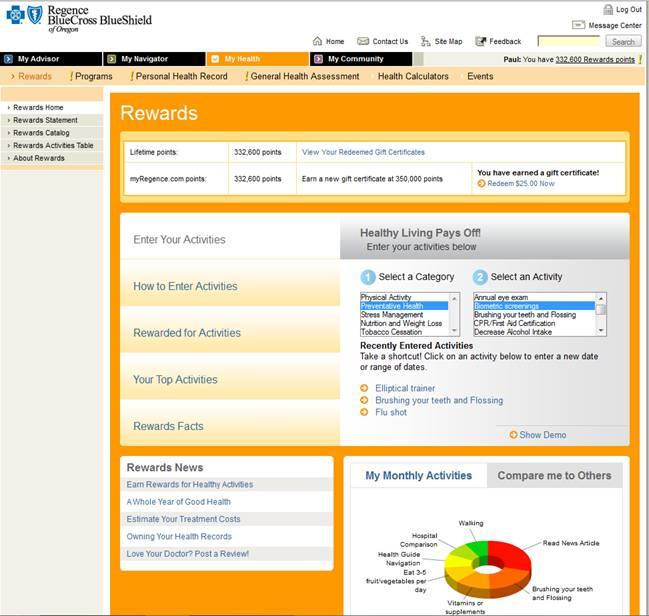 Regence Program Rewards Transformational Activities
Regence Program Rewards Transformational Activities
Regence started on a new path to consumer engagement back in 2005.
After seeing a recent presentation outlining their consumer engagement framework, I reached out to Torben Nielsen, VP, eBusiness Strategies and Services at Regence to learn more. Torben shared their past journey as well as their future direction with me.
Here are the 4 steps along their consumer engagement path. Regence is currently at Step 3 and has a conceptual view of their next step which will continue to evolve as the market landscape fills in around them.
Consumer Engagement Step 1: Know Me
Regence’s first step focused on the passive cardholder, giving them value as they logged in. The cardholder saw all of their claims, benefits and provider information. This was back in 2005. Prior to that “it was not a good experience” since the member only saw some of their claims information and the list of providers “did not even indicate whether each one was inside or outside their network”.
Consumer Engagement Step 2: Engage Me
Beginning in 2008, Regence decided that they needed to get to know their members in order to effectively engage them.
Instead of linking the member over to their health or wellness program vendor’s website, Regence decided to keep the member within their portal to capture their online behavior.
Around that time, Regence launched their Rewards Program which awarded points to members for “tranformational activities”. These activities were rewarded because they “informed, empowered and educated the consumer”, including looking up content around a health issue or participating in a wellness program. Regence decided not to reward members for “transactional activities” such as looking up a claim or searching for a provider. Regence really needed to keep the member on their portal to track their online behavior in order to reward them.
Next Regence started their email program, sending out relevant electronic communications to bring members back to the site. Although many health plans have an interest in emailing members, I hear all the time that they do not have their email addresses. Regence collects the member’s email address during their site registration process. “We can’t engage with out email. It would be a missed opportunity to get in front of the member”, Torben emphasizes.
In addition to generating additional portal traffic, health plan communications can also strengthen their member’s satisfaction scores, which is more important now than ever with the increased market competition.
Consumer Engagement Step 3: Connect Me
Over the past two to three years, Regence has been moving faster down the path with consumers.
“Connect Me” goes beyond the “member to health plan” relationship. According to Regence, this also includes strengthening the “member to member” bond through social community and the "member to their care team" bond through ACO efforts.
One important way for Regence to strengthen the “member to member” relationship is by getting consumers to contribute more content online through conversations, ratings/reviews and suggesting local events in their geography.
Another aspect of “Connect Me” addresses the cross communication channel experience since members are increasingly accessing and engaging through their mobile devices. “We’re connecting the data that we’re sitting on to provide a more personalized experience for our members”, explains Torben.
Consumers are engaging with Regence!
- 67,000+ patient reviews have been submitted by members, of which 90% are favorable (i.e. the member would recommend the physician/facility).
- 63,000+ posts in the Community section of myRegence.com, written by more than 6,000 unique content creators.
- 346,000+ have opted- in for member electronic communications (e.g. updates and alerts, account information, etc)
- 260,000+ subscribers signed up to receive the bi-weekly myRegence.com email newsletter
Consumer Engagement Step 4: Partner with Me
As they look down their Consumer Engagement path, Regence has determined where they want to be directionally. Regence wants to be relevant to the consumer’s every day life. Something consumers need to check as part of their daily routine. Their starting place to look for information to meet all of their health needs.
Although it is challenging to know exactly where the market is going, Regence will remain in touch with their users to help guide the way.
In fact, Regence has over 400 users that help advise them by providing ongoing feedback to potential directions. [Note: Innovative companies have consumer advisory boards as a best practice. Increasingly, these consumer advisory boards are managed in a private online area and the insight captured is used to guide product and marketing decisions.]
Regence is co-creating with this growing group of consumers to define and refine online capabilities. When Regence asked for feedback about “patient reviews”, members felt they needed to see more than the reviewer’s screen name. Users wanted “the ability to connect with their peers in order to get advice when selecting a provider”. In the latest patient review experience, the screen name is linked to the reviewer’s Community profile page, where to learn more about who they are, where they’re from, what they do for a living and members have an the opportunity to make a friend request.
Regence’s Results Realized
Due in large part to Regence’s consumer engagement strategies, myRegence.com experienced the following results in 2011 over 2010:
- 30% increase in the cumulative number of content creators (i.e. those who have left a patient review, posted in Community or both).
- 88% jump in the number of $25 gift card redemptions through the Rewards program
- 76% increase in the Consumer Engagement Index (CEI) which measures the user adoption of transformational features
- 26% open rate for targeted email campaigns, nearly 2x the industry benchmark of 14%
Regence has also noticed that their segmentation efforts for email have been effective in engaging consumers. For example, by sending a Patient Review email to previous reviewers, Regence realized a 38% open rate.
As Regence moves onto step 4 in Consumer Engagement, they are conceptualizing new ways to reach out to their members with relevant information from their plan, community and care team. And they will be innovating with and listening to their users throughout their journey.
Seven Strategic Directions for Engaging Employees Through eHealth
 July 21, 2011
July 21, 2011  RedBrick Health Employees Participating in the Biggest Loser Minnesota ChallengeDuring the Healthcare Unbound conference in San Diego last week, I started our “New Directions in Employee Engagement” panel with an overview of innovative approaches that are emerging.
RedBrick Health Employees Participating in the Biggest Loser Minnesota ChallengeDuring the Healthcare Unbound conference in San Diego last week, I started our “New Directions in Employee Engagement” panel with an overview of innovative approaches that are emerging.
1. Employee Driven. Companies are moving beyond surveys and focus groups, which gather a snap shot of insight, to co-creating with their employees in a private online community. Within their intranet, these employers are enabling their employees to surface new ideas, define new products and programs suggested by co-workers and prioritize where they want their employer to invest their limited health and wellness resources. During the conference panel, Lisa McGill, VP, Worldwide Human Resources from Brocade, discussed their online BHive community where their WellFit Employee Advisory Council innovates on wellness offerings.
2. One Integrated Program on One Platform. Employees struggle every day to keep their job, family and personal life on track. Instead of promoting many separate ways for their employees to pay attention to their health, companies are bringing all their initiatives into a single and integrated program. Employers are tying their health risk assessments, screenings, social challenges and coaching in with their reward program to incentivize their employees. At the same time, they are simplifying the process with an integrated technology platform. With this holistic approach, employers are able to monitor the elements of the program that are driving healthy change while experimenting with new elements such as mobile applications to generate engagement.
3. Customized Approach. “My employees work in a call center and do not have time to attend our onsite wellness sessions but would be interested in watching a webinar for example around stress management”, explains a large technology employer. The key to engaging employees is to understand their lifestyle profile and customize a program that fits into their day and aligns with their technology comfort. Think about how different the Health & Wellness Program may be for a technology firm than a manufacturing company. One size does not fit all.
4. Personalized Experience. Some of the biggest mistakes that employers are making is distributing all of their content to all of their employees or assuming that one area (e.g. walking programs) appeals to all of their employees. More innovative employers are enabling each employee to determine how they want to participate based on their interests and needs. These employers are also letting their employees set their content and communication preferences which guide their multi-channel experience.
5. Influencer Enabling. With the emergence of social health related challenges within a company and the associated online social network to connect teammates, employers are noticing that certain employees are having a positive impact on the health behaviors of others. Employers are starting to arm these influencers with online tools and resources. Some companies are calling them “Wellness Ambassadors” or “Wellness Champions”. Employers that have many different offices with limited budget are leveraging these influencer representatives to generate engagement throughout their company footprint.
6. Social Currency. Employers are letting their employees create social currency by providing a space on the intranet to share. Employees are uploading pictures, videos and writing stories such as how Susan lost 50+ pounds or when Joe participated in his first triathlon. Why is this social currency valuable to employees? It is inspirational, insightful and meaningful since these contributions are from fellow employees with whom they have a common bond. This social sharing is particularly powerful when an employee turns their experience into a mini- challenge to other employees. Bryce Williams, Director of Wellvolution, Blue Shield California mentioned that throughout their 6- week employee social competition, there were “over 1,000 viral wellness challenges”.
7. Family Engagement. “We are trying different approaches to get the spouses to participate in our health programs,” explains a large financial services employer. Employers are extending rewards to the spouses to motivate their participation. This is particularly important since employees make many health and wellness decisions on a daily basis with their spouses and we all know that negative behaviors can be costly. How are employers engaging with families in a positive way? During the panel, Pat Sukhum, Co-founder and Marketing Director at RedBrick Health described their Biggest Loser Challenge which this year was extended to the community and to employee’s families. “One of the largest divisions in Challenge included over 3,400 participants who signed-up as teams of families to compete and improve their health together,” Sukhum noted.
Each of these new directions in employee engagement requires a technology solution to power the capabilities described. Given that each employer and set of employees is different, it is important to determine what is needed and how to tune the solution to deliver the communication, collaboration and challenges to engage employees and their families.
Secrets for Leveraging Social Community for Member Engagement
 November 16, 2010
November 16, 2010 During the 6th Annual World Technology & Innovation Congress (WHIT), I led a panel to share Social Community insights from The Regence Group and Blue Cross Blue Shield of Rhode Island. With my extensive online community experience, I was impressed with the capabilities and design of this healthcare social community that Regence has built and grown to over 600,000 members across five Plans and four states.
Torben Nielsen, Director of myRegence.com has been leading the community development from the beginning, incorporating features to engage the member such as rewards, ratings, decision support tools and an integrated experience tying together content into community.
Key Concerns for Social Communities
As health plans develop their social community strategy, they often confront three key concerns from internal stakeholders. The first is around addressing negative comments by members. “We tell them that your members will say what they want about your plan but you have an opportunity within the community to have a customer service contact them directly to resolve any issues or post a response to their comment”, explains Torben. A second concern is about the posting of personal health information which can be filtered by the community software. The third issue is about consumers offering inaccurate information. “One of the roles of our moderators is to ensure that the member is directed the right answers when necessary”, replies Torben.
Engagement Capabilities within the Community
The Regence group designed MyRegence.com with a compelling set of features to engage and empower members. Here are four capabilities that I feel are the most compelling:
1. Reviews. This social community requires that you have a claim before you can review your provider experience. Your provider can post a response to your comments following your review. Other community members can send you a message to learn more about your experience as they consider using the provider.
2. Rewards. Members earn rewards points for using the Community to review new health information, become part of a wellness group and for entering their wellness activities such as exercise, diet and preventative care.
3. Decision Support. As a member considers a particular treatment option, he can review the percentage of members who have had the treatment done or prescribed and see the estimated treatment cost range and an estimated personal cost.
4. Integrated Experience. When a member reads information about eating healthy, she can click a link to watch videos from Chef Tse, discuss ideas for cooking light meals with the community and request to receive eNewsletters filled with food related articles and links into additional content and community discussions of interest.
My Blue Community
The Regence Group has defined a part of my Regence.com as the My Blue Community to serve as a national online community platform that supports members from other participating Blues plans including early adopters Blue Cross Blue Shield of Rhode Island, Blue Cross Blue Shield of Massachusetts and Blue Cross Blue Shield of Louisiana. Kimberly A. Holway, Market Segment Manager, Strategic Marketing & Product Innovation from Blue Cross & Blue Shield of Rhode Island discussed their experiences planning and rolling out My Blue Community to their members this past summer.
Value Proposition to Members
“When we marketed My Blue Community to our members, we positioned it as a ‘safe and secure place to share experiences and get support’ from others”, explains Kimberly. “We view this as a way to expand the network so that members can more readily find people with their same health issues and interests”. BCBS of Rhode Island members are expressing the value that they see with the community. One member confirmed that it was a ‘safe environment to seek advice’ with peers that are ‘trustworthy’.
As Torben pointed out, you need to be a member of the health plan to log in which ensures that they are an adult participating in the community.
Another BCBS Rhode Island member expressed the value that she gains ‘by reading what other people have posted’ and ‘seeing stories which are relatable’.
Member Engagement Validation
There is so much to learn about how consumers engage in private vs public (e.g. Facebook, destination health sites) social communities. Healthcare organizations are experimenting with both formats to understand the differences in the content shared and the frequency that consumers engage just to name a few. When evaluating engagement, it is also important to understand how much consumers gain when contributing vs consuming content from these communities.
How can health plans bring new sources of value to educate, support and enable members to collaborate with others about their health within these social communities? Stay tuned.