Permalink
Permalink St Lukes Health Expands Patient Access through Integrated Virtual & Hybrid Care Model
 June 25, 2024
June 25, 2024 
During the recent Home & Hybrid Care Virtual Summit 2024, St Lukes Health shared how they have expanded virtual access to support patient care journeys over the past three plus years. It is refreshing to see how St Lukes views virtual as a big front door to their care network, how they have personalized the entrance and experience across more than a half dozen patient programs and how they have invested in an integrated data platform and tools for better care experiences.
Like other health systems, Idaho- based St Lukes Health is addressing today’s healthcare headwinds including staffing challenges, provider burnout, the consumers increased expectations for their healthcare experience, all within the regulatory and reimbursement landscape.
In September 2021, St Lukes Health launched a telehealth program to patients with one of seven low acuity conditions. Since then, their virtual program has expanded to provide patients with immediate care access until they can schedule and see their providers, which may take up to a few months.
“Our team value is that we (virtual care) will be the quickest access to a provider”, explains Abby Losinski, MHA, Director of Telehealth at St Lukes. Abby’s group is part of the Consumer access and experience team.
St Luke Virtual & Hybrid Model
Since late 2021, St Lukes has developed needed processes and infrastructure to successfully expand their virtual program with a centralized virtual support team, virtual command center platform to address incoming patient demand and virtual care patient data integration to support care collaboration and a superior patient experience.
While many health systems launch separate virtual programs to support urgent care, mental health, and chronic conditions, St Lukes centralized team supports many patient populations with virtual care access. They view this virtual interaction as an opportunity to begin a patient relationship.
Several patients targeted by St Lukes for their virtual care program:
- New Patients (December 2021) St Lukes promoted virtual services to welcome patients without a doctor but with an immediate need. During the virtual visit, patients can refill a prescription, get scheduling help and access care support until their appointment. Patients needing a higher level of care are quickly connected with a clinician.
- Urgent Care (May 2022) Patients at St Lukes’ Urgent Care Centers with high wait times are offered a virtual appointment when they meet certain criteria. Patients use their mobile phones for the visit and are urged to stay nearby if point of care testing is required. This gives patients a chance to be seen when there are no available rooms.
- Service Line Extension (January 2023) “We are an extension of any department where patients need same day access” (e.g. primary care, urology, oncology, pediatrics) explains Losinski. “We work with the Medical Directors to build clinical guidelines so that patients are treated the same way whether they are coming in to see a specialist or meeting with our virtual clinician”. Losinski is proud that St Lukes “can offer multi-specialty care from one centralized team”.
- Maternity/New Pregnancy (April 2023) After learning about their pregnancy, patients often have questions and concerns. Instead of waiting for their first appointment which may take 8-10 weeks, patients can meet with a clinician virtually and set up notifications in MyChart to immediately receive information about their maternity care and growing baby. During the virtual visit, patients can get scheduling help and care can be escalated if required.
- Home & Community Access (Sept – December 2023) St Lukes has set up “virtual hubs” enabling patients to connect virtually using digital health tools from a partnership with TytoCare. “We wanted to expand what we can treat virtually because we have new tools. If we can’t see into the ear, we can’t treat it” and the revenue is lost, Losinski explains. St Lukes now offers TytoCare Home devices (e.g. otoscope, stethoscope, throat camera, skin camera) to patients at home and TytoCare Clinic to patients at schools, libraries and workplaces, to capture data for the virtual care team decision support.
St Lukes Virtual Care Access Experience Success
Their virtual program success is achieved through continuous focus on the patient experience. St Lukes has designed their virtual experience from the outside- in and offers patients the bridge into their health system care network.
Here are several success elements that I have noticed to deliver care continuity:
Designed Patient Experience to fit care scenario. Newly pregnant patients are set on the Maternity path, supported by the virtual team with education, testing and virtual visits until their OB appointment. Service Line Extension patients such as oncology may have access to digital tools for remote monitoring with condition education and support until their specialty appointment.
Partnered for Patient Care Coordination. St Lukes’ Consumer access & experience team has built partnerships with different service lines and settings across their network. Patients accessing virtual care at St Lukes needing more care are escalated to these clinical partners within the St Lukes network. St Lukes ensures patient care quality is maintained by using the same clinical guidelines for virtual and in- person care.
Built Integrated Patient Data & Tech Infrastructure. “St Lukes has decided that virtual care can not be this thing that lives outside of the health system”, Losinski emphasizes. St Lukes has invested to integrate and augment patient data (TytoCare devices) enabling clinicians to access information from all clinical interactions and from patients from beyond the walls to deliver better patient care and experiences.
St Lukes Virtual Care Feedback
Through marketing research, St Lukes has learned:
Consumers: The “brand” offering virtual care services really matters. Consumers like that the doctors conducting the virtual visits work for St Lukes and live in the community and appreciate that their PCP can view their virtual visit notes.
Patients: After participating in St Lukes’ virtual services, patients rated the experience an equivalent of 4.9 stars (out of 5). “Thank you for being there when no one else was” shares a patient.
Providers: Clinicians delivering virtual services have a strong provider experience; “appreciate the increased location and schedule flexibility”, “being in the moment for patients” and “getting to work from home”.
St Lukes Virtual Care Direction
Earlier this year, St Lukes launched eVisits, an asynchronous virtual care option. For $29/visit, patients can message a clinician about one of seven symptoms. eVisits are viewed as a virtual care “entry point which affordable and convenient for patients”.
St Lukes will continue expand virtual care access for their patients. “Currently, we are 8am-8pm but we are looking to extend our hours to 24x7” Losinski shared.
It is impressive to see how St Lukes brings patients into their care system through a larger virtual care front door, leverages care partnerships and protocols for consistent patient care quality and empowers care collaboration with integrated data and tools. St Lukes’ virtual care investments and vision enable them to effectively address staffing and consumer expectation challenges while delivering a superior patient and provider care experience.
Stanford Health Care Elevates Patient Experience with Design Thinking
 September 5, 2023
September 5, 2023  Navigation Bar for Stanford Health Care Patients“Healthcare today is changing and we need to be a catalyst for change with our patients,” explains Alpa Vyas, Stanford Health Care’s Chief Patient Experience & Operational Performance Officer. “In order to create a superior experience for our patients, we have expanded our understanding of patient needs through empathy, incorporating design thinking into our clinical and operational processes."
Navigation Bar for Stanford Health Care Patients“Healthcare today is changing and we need to be a catalyst for change with our patients,” explains Alpa Vyas, Stanford Health Care’s Chief Patient Experience & Operational Performance Officer. “In order to create a superior experience for our patients, we have expanded our understanding of patient needs through empathy, incorporating design thinking into our clinical and operational processes."
As part of Stanford Medicine, Stanford Health Care has a long history with patient experience and is committed to continuous improvement by collaborating with patients on products, programs and processes. Patient Experience is one of Stanford Health Care’s four main pillars, demonstrating the importance to their organization.
At the PX Symposium in Boston, Alpa will be presenting Design Thinking Rx: A Prescription for Innovative Healthcare Solutions. Join me at the Symposium to learn more about Stanford Health Care and other truly patient- centered organizations. I will be leading a round table discussion to exchange best practices and processes for a superior patient experience.
5 Questions in 5 mins, Interview by Sherri Dorfman, MBA, CEO Stepping Stone Partners
1. How do you define Design Thinking at Stanford Health Care? How does this fit with Human- Centered Design and Co-creation?
“We view Design Thinking as the ‘How’ we problem solve. We start with the end user/patient and use empathy to gain insight into needs to define the problem. Then we move through the Design Thinking process with ideating, prototyping and testing solutions.
We see Human Centered Design as the ‘What,’ our philosophy of engaging with the patient at the center of our process. Co-creation is the ‘Who’. We collaborate internally with our physicians and staff and externally with our patients.”
2. Tell me how Stanford Health Care gathers and leverages insights during the Design Thinking process.
“We use a ‘Collaboration Model’ where we define the problem statement and then refine it with insights collected from internal (e.g. clinical, operational, technical) and external (e.g. patients, family caregivers) stakeholders. We use surveys, discussions and observations. Depending on the project, our internal discussions may point us to others with specific expertise or experience interacting with patients. For patients, we may observe them (with their permission) in the hospital or their home to understand their needs for care and support.”
3. Can you share an example of how Stanford Health Care has successfully used the Design Thinking process to define a better patient experience?
“We are in the process of enhancing the service that our ground navigation team delivers and are excited about what we have discovered. We want to move beyond typical wayfinding services and hospitality approach. Through discussions with our operational leaders interacting with patients who are looking for information and guidance, and via patient surveys and interviews, we learned about the need for improved communication support and better coordination support. We are defining a new, higher level navigation role which will allow us to expand and enhyance our level of patient support. This may include scheduling appointments post discharge from an inpatient unit or emergency department, arranging transportation, securing lodging for family members and providing care updates on for patients – For example, ‘I spoke with the nursing team and they will be bringing you back in 20 minutes’.”
4. Thank you for that specific use case. Tell me how Stanford Health Care is using Design Thinking to address a broader patient problem.
“During the pandemic, we had to pivot on how we provided care ‘Access’ to our patients, from in -person to virtual visits. Looking forward, we want to start thinking about ‘Access’ differently. We are engaging staff and patients in the process of defining the next generation of care, including asynchronous care. We are learning that patients see care ‘Access’ as much more expansive. Based on insights from staff and patients, we are exploring some ideas including PCP eConsults (curbside) with specialists to determine the need and urgency for the appointment and virtual nurse triage.”
5. How does Stanford Health Care measure success for PX initiatives?
“Back in 2022, I contributed to a PX Journal article called ‘Measuring what matters: A proposal for reframing how we evaluate and improve experience in healthcare’. Through extensive discussions with industry experts, the journal article concluded that in order to design experiences that are meaningful, we need to understand what really mattered to patients, families and care partners. At Stanford Health Care, we have looked at our surveys where we ask the same questions and engaged with staff and patients for their feedback. With those insights, we have added questions including those to get feedback on new process enhancements.
We are bringing these survey and discussion insights (including open ended comments) to our operational team members in real- time to translate into immediate changes for our patients.”
With planning underway for 2024, Alpa and her team are interested in further utilizing Design Thinking to develop better programming for Stanford Health Care. “We are working on the next generation of care- exploring ways we can use the insights we have gained to create more personalized experiences for our patients. The Design Thinking process will guide our exploration on how to leverage data and feedback that may be buried within our systems to hone in on specific challenges and solutions – this is where we hope to invest”, Alpa concludes.
 Permalink
Permalink Providence Saint John uses AI platform to Empower Cancer Patients & Providers for Better Care
 July 20, 2023
July 20, 2023  In October 2022, Providence Saint John's Health Center invested in Project Ronin, an AI driven cancer intelligence platform to empower cancer patients and their clinical teams to manage treatment symptoms, care communications and clinical decision support. Their goal is to reduce ED visits and deliver better patient care and outcomes.
In October 2022, Providence Saint John's Health Center invested in Project Ronin, an AI driven cancer intelligence platform to empower cancer patients and their clinical teams to manage treatment symptoms, care communications and clinical decision support. Their goal is to reduce ED visits and deliver better patient care and outcomes.
According to the American Cancer Society’s 2023 Cancer Statistics report, cancer remains the second highest cause of death after heart disease. This is an estimated 2 million newly diagnosed cancer cases resulting in about 610,000 deaths.
Dr. Martin, MD, CMO of Providence Saint John’s believes that providing a new “space where cancer people can engage with their physicians has some very real, tangible benefits.” The digital tool is designed to support “patients with less-critical symptoms, which has the potential to reduce emergency department visits and improve clinical efficiency, which means a more efficient utilization of resources. Of course, we always advocate patients to come to the emergency department if they believe they are experiencing a medical emergency.”
Cancer Care Collaboration
Successful treatment of cancer is multifaceted, requires a multi-disciplinary care team, entails managing different data sets with continuous capture and monitoring of data, and has data complexity given the non-linear nature of the disease (i.e. diagnosis, treatment, remission, recurrence, treatment, survivorship/death).
Patients struggle to manage their cancer, both mentally and physically. Patient treatment symptoms can be severe. Questions come up between treatments but care teams are extremely busy. Patients need to remain connected to care teams to stay engaged, better manage, and communicate side effects.
Providers try to navigate their inefficient clinical workflows, address the administrative burden due to documentation requirements, and deal with workforce shortages. Today, providers spend 20-40 minutes finding patient info to prepare for patient visits, sometimes missing key data. Providers are overwhelmed to make needed decisions for cancer patients at the point of care.
AI Cancer Platform Delivers Care & Decision Support
The Ronin Cancer Platform enables patients to “take control of their care in a way that wasn't possible before and feel better connected to their care teams,” explains Dr. Neil Martin, MD, CMO of Providence Southern California Clinical Institutes and Executive Director of Saint John's Cancer Institute. Clinicians utilize this cancer intelligence platform’s predictive analytics and clinical dashboard to define treatment pathways and support more informed care decisions.
How does this work? The Ronin cancer platform takes structured and unstructured data from different EHR silos, and then cleans, calibrates, contextualizes this information to present care insights. With predictive analytics, providers can identify at-risk patients and see a complete real-time view of the care journey for immediate actions.
AI Data- Driven Cancer Platform: Patient Experience
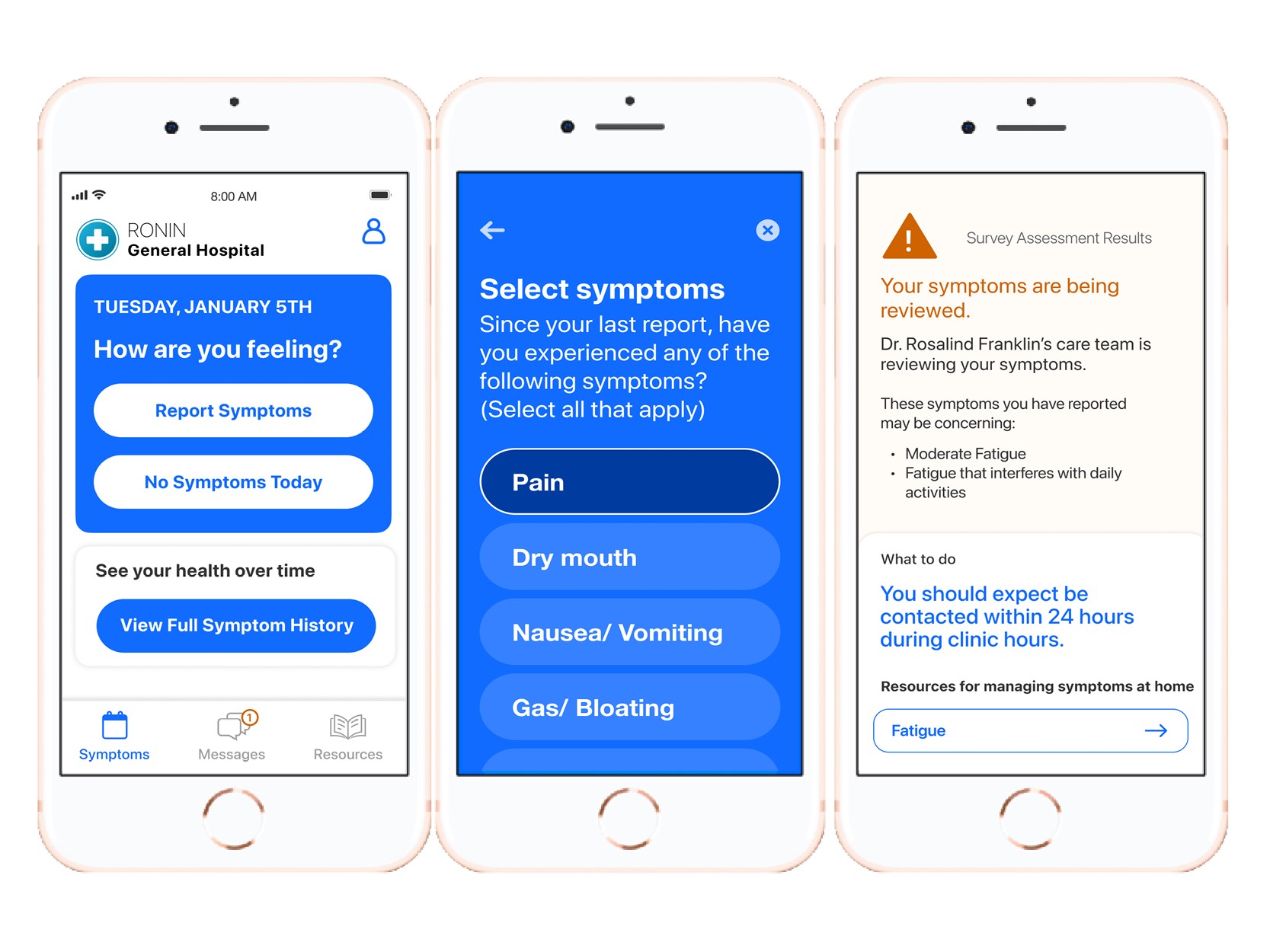
Patient Patricia (patient persona), 74 years old, is newly diagnosed with breast cancer. While meeting with her new care team, Patricia learns about new resources including the free Ronin Symptom Monitoring App, to educate and support her as she navigates her cancer path. During her next appointment, Patricia notices the poster in her doctor’s office prompting her to download this patient app.
Patient Symptom Monitoring App Poster:
We want to support you through your treatment. In between your visits, please let us know how you're feeling by using the Ronin Symptom Monitoring Application. This will help us catch any side effects that you may experience. Studies show that symptom monitoring can ...
• Help people live longer and improve their quality of life
• Help people stay on treatment longer
• Lower visits to the emergency room and reduce hospital stay
Patricia downloads and begins using the Symptom Monitoring app which captures her Patient Reported Outcomes (PROs), enables her to track and manage side effects for treatment tolerance, displays her symptom history and provides her with personalized education based on what she is reporting. Within the app, Patricia selects from a list of symptoms and then sees a message that her symptoms “are concerning”, that her care team is monitoring this and will reach out to her within 24 hours.
AI Data-Driven Cancer Platform: Provider Experience
Patricia’s care team receives a “symptom alert” through the EHR based on the information that she has entered. Her symptom information has required a response (e.g. new symptom, moderate or severe symptom). The Nurse Navigator reaches out electronically or telephonically to check in on Patricia to understand more about her symptoms.
When her Oncologist Dr. Davis initially set up Patricia’s personalized care pathway on the platform, he indicated her specific disease type, which triggered patient reported outcomes surveys and at-risk surveys which captures data and intelligently prioritizes for the care team to take quick action to course correct and preempt adverse events.
While preparing for an upcoming office visit with Patricia, Dr. Davis uses the Ronin Platform to view a longitudinal timeline of her cancer journey, filled with real-time data (e.g. labs, images, pathology, treatment, surgery notes, past encounters) to make informed, proactive and personalized treatment decisions. Following the visit, Dr. Davis (or the clinical staff) pushes educational content to help Patricia to navigate her new symptoms or cancer stages.
AI Driven Care Experience Value Proposition
At Providence Saint John's Health Center, both patients and providers are finding value using the AI Ronin Platform, including clinical efficiencies, better care and outcomes and higher satisfaction. Here are some comments from the patient and provider users:
Patient Experience:
“Ronin provided confidence someone was monitoring me.”
“Ronin made me feel like my care team was with me, even at home.”
“I prefer not having to call the hospital. (With app) I am able to record side-effects right away as they are happening”.
“It’s (app) so easy to open up and write how I’m feeling…It’s a great reminder to me that even though I may think I’m fine, I need to pay attention to my symptoms.”
Provider/Staff Experience:
“We were able to catch an immune- related toxicity early for a patient of mine. Without Ronin, I would not have caught it”. Medical Oncologist
“We want to make sure the patients are having the best quality of life. With Ronin, we can check in on them more frequently.” Nurse Navigator
“From the treatment team’s standpoint, it’s made it easy to follow patients. It’s a great way to stay hands-on.” Nurse Navigator
“I had a patient straight up tell me ‘If it wasn’t for the app, I would be calling you guys every day'.” Medical Oncologist
“Visually, the Timeline tab makes it much easier to get up to speed on a patient. Especially compared to reading my colleague’s last notes.” Medical Oncologist
Success Metrics
In addition to gathering qualitative comments about the patient and provider/staff experience, Providence Saint John’s tracks quantitative success metrics for the AI driven Cancer Program. Some key metrics include:
● Reduced unnecessary ED admissions by >20% (early findings)
● Improved efficiencies with 35% decreased patient call volume and 32% patient-initiated messages.
● Strong patient satisfaction & experience
- 84% see positive impact on care experience
- 90% say app is easy to use
- 88% are satisfied with solution
Future for Providence with Ronin Cancer Platform
Moving beyond the patient mobile app and care communication from phase one, Providence Saint John's is planning to provide clinical decision support with oncology and risk dashboards and the capability to view comparative patient analytics in phase two.
"We are proud to implement evidence-based care solutions for patients in our community," said Brad Bott, Executive Director of the Southern California Clinical Institutes. "Our partnership with Ronin will help improve cancer care delivery while empowering our staff to practice more efficiently. It's a win-win."
Ochsner Health System’s Digital Medicine Program Success
 January 12, 2023
January 12, 2023 Digital Medicine is a nationally recognized, clinically proven program revolutionizing how we treat chronic conditions combining digital tools and engagement with a dedicated care team.
 Ochsner O Bar Supports Patient's Digital Health needsIn 2015, Ochsner Health launched its first Digital Medicine Program for Hypertension. Since publishing success outcome measures in The American Journal of Medicine, Ochsner’s Chief Clinical Transformation Officer Dr. Richard Milani, and his team have built on the framework to support patients with chronic conditions (e.g., Diabetes, COPD) and Maternal care. Over 30,000 patients have participated in an Ochsner Digital Medicine Program.
Ochsner O Bar Supports Patient's Digital Health needsIn 2015, Ochsner Health launched its first Digital Medicine Program for Hypertension. Since publishing success outcome measures in The American Journal of Medicine, Ochsner’s Chief Clinical Transformation Officer Dr. Richard Milani, and his team have built on the framework to support patients with chronic conditions (e.g., Diabetes, COPD) and Maternal care. Over 30,000 patients have participated in an Ochsner Digital Medicine Program.
With the cost of chronic care, including indirect costs (productivity loss) reaching $3.7 trillion a year, Ochsner is focused on better managing chronic care through three key levers: medication management, behavioral change, and frequent data collection from home.
Milani believes that a successful Digital Medicine Program must:
- use the latest guidelines for medication management, important because ideal medications are always changing, and a certain medication may be more effective for one patient (profile) than another.
- be designed with behavioral science to impact lifestyle change, which includes everything from delivering the right type and timing for nudges to aligning patient needs with right level of high touch care support.
- leverage data captured and presented within a reasonable time so that clinicians can respond before the patient’s health becomes a problem.
Dedicated Team, Centralized Monitoring
Ochsner’s Digital Medicine programs are supported by a dedicated team of over 60 professionals, including clinicians, coaches, pharmacists, physical therapists, behavioral scientists, IT developers, technology engineers, user experience, content specialists, data scientists and advanced analytics.
Team members help patients throughout their program journey, with onboarding, educating and ongoing care support. An important benefit of having one Digital Medicine team is that the program can be personalized to the patient’s specific needs (e.g., required monitoring devices) and supported by the same clinician and coach.
EMR Foundation
“The technology foundation of our Digital Medicine Programs is the EMR Epic,” explains Milani. “Our patients are given clinically validated devices approved for the program, with device data flowing into the EMR.”
Ochsner has evaluated and selected a set of devices for this program for each condition, which patients are required to use to connect into the Program. Ochsner distributes the devices and is the point of contact for any technical issues.
Patients access their Digital Medicine Program through the Epic portal My Chart (via website and patient mobile app), where they can view trends on device measures, access educational information, complete assessments, and exchange messages with the Digital Medicine Care team.
“For our clinicians, we have designed dashboards which help triage and prioritize patients based on incoming patient health data including Social Determinants of Health,” says Milani “We have set up alerts for our program care team based on selected physiological and inputted measures. Other providers of the patient’s care can access information in Epic, including a Monthly Report.
Patient Digital Medicine Program Experience
 Ochsner Digital Medicine Patient After a referral from his physician, patient Peter (not his real name) is invited through Epic to participate in Ochsner’s Hypertension Program. Participating in the program means that Peter can reduce time off from work and save time driving time for some appointments.
Ochsner Digital Medicine Patient After a referral from his physician, patient Peter (not his real name) is invited through Epic to participate in Ochsner’s Hypertension Program. Participating in the program means that Peter can reduce time off from work and save time driving time for some appointments.
Peter has the option of having the device(s) and program setup information mailed to him, or if nearby, Peter can stop by Ochsner’s O Bar – a physical location that allows patients to test drive more than 100 Ochsner-approved health apps and purchase devices. There’s a technology specialist behind the counter to answer questions and give app demonstrations. (Think genius bar to support patient health technology).
Once Peter sets up his blood pressure monitor, his measures are sent to his care team. If any measures are out of range, his care team will reach out to discuss any possible changes needed. Peter’s coach sets up personalized messages regarding lifestyle changes needed and reminders to keep him on track with taking his medication and taking his readings. Peter can communicate with his coach via SMS texting, My Chart messages or via phone.
“We are seeing that patients prefer to communicate asynchronously with their clinicians and coaches, so we are giving them the tools to do so,” says Milani.
Digital Medicine Program Success
“We evaluate success based on a few key measures,” says Milani. “We look at outcomes and are seeing a consistent 2-3 times improvement in control rates with our program. We also look at Net Promoter Scores (NPS) and we are getting very high patient satisfaction scores of 87-90.”
Ochsner recently conducted a pilot program (beginning in June 2020 and ongoing) to investigate how digital medicine with remote patient management can improve outcomes for Medicaid patients battling chronic diseases like Hypertension and Type 2 Diabetes. The results were statistically and clinically significant. Enrollment in Ochsner Digital Medicine brought nearly half of all out-of-control Hypertension patients under control at only 90 days, which was 23% more likely than usual care. Control rates continued to improve as patients remained in the program during its first 18 months. More impressively, 59% of people with poorly-controlled diabetes achieved control over their condition as part of the digital program – a rate twice as high as usual care.
Most patients achieved control of their hypertension and diabetes within 90 days of beginning the program, even those who had poor control prior to enrollment.
In addition to improving health outcomes, participation in the digital medicine program resulted in high patient satisfaction, with a net promoter score greater than 91 for Medicaid participants. This is consistent with the high patient satisfaction with digital chronic disease management programs at Ochsner among non-Medicaid patients.
“We're offering patients compassionate human care combined with the power of technology, and we’ll continue to expand these programs to help more patient populations”, Milani concludes.
Success in their words
Patients:
“My care team has been really helpful. They’ve explained things to me… offered me suggestions. I really like the fact of daily accountability. I’ve lost about 103 pounds. I feel better. I have energy that I didn’t have a year ago.”
“I know I’m sleeping better–my hair, my skin, my vision–just different things that you start to notice that we take for granted that are all tied into our blood pressure and blood sugar. I’m a living testimony that it (the program) works! I know for a fact Ochsner Digital Medicine has saved my life.”
“I feel like this is more normal. Someone’s got my back and… I will be able to use [the program] for the rest of my life.”
“The Ochsner Digital Medicine Care Team helped me by guiding me in every way possible – giving me tips on my diet and adjusting my medication on the fly. They are a good support team.”
Staff:
“I love the Ochsner Digital Medicine program. As a physician, I love having the Digital Medicine team helping me because it’s like having other coaches on the team.” Dr. Victoria Smith
Ochsner’s Digital Medicine Program is available to employees across their health system.
“The Ochsner Digital Medicine program is one of the most important components of healthcare for our (employees). If I can offer better benefits and possibly reduce healthcare costs, why wouldn’t I? We have had employees sign up for the hypertension and Type 2 diabetes programs and have seen many positive results in a short period of time. The program lets your employees know how much they mean to you by investing in them”, Chief of Administration, Chris Kaufmann
 Permalink
Permalink  care collaboration,
care collaboration,  chronic care management,
chronic care management,  patient generated health data in
patient generated health data in  Behavior Change Health & Wellness,
Behavior Change Health & Wellness,  Care collaboration,
Care collaboration,  Connected Health,
Connected Health,  Decision support,
Decision support,  Mobile Health,
Mobile Health,  Patient Centered Care Design,
Patient Centered Care Design,  Patient Decision Support,
Patient Decision Support,  Patient Engagement,
Patient Engagement,  Patient Experience,
Patient Experience,  Patient Journey,
Patient Journey,  Patient Portal,
Patient Portal,  Population Health,
Population Health,  Population health management,
Population health management,  TeleMedicine,
TeleMedicine,  digital health,
digital health,  online coaching,
online coaching,  patient health education
patient health education New England Baptist Hospital Hip Replacement- Patient & Caregiver Experience
 June 9, 2021
June 9, 2021  Beginning Surgery ExperienceTwo weeks ago, Sam had hip replacement surgery at New England Baptist Hospital, a top nationally recognized orthopedic facility in Boston.
Beginning Surgery ExperienceTwo weeks ago, Sam had hip replacement surgery at New England Baptist Hospital, a top nationally recognized orthopedic facility in Boston. - Orientation Timing: The virtual meeting was within a few weeks prior, so this gave us ample time to prepare in the days leading up to his surgery date.
- Orientation Content: The hip surgery nurse specialist reviewed pertinent information about what to expect before, during and after the surgery. The follow up emails including “Planning for your Recovery” provided essential information to get Sam’s home ready for his return post-surgery, addressing fall risks.
- Individual Patient & Caregiver Consultation: Since we had some questions that were specific to Sam’s situation, I wish that we had the option to schedule a virtual visit with the nurse to address our concerns in the days leading up to surgery. This would have reduced our anxiety around what to expect Sam to be able to do at different points of recovery.
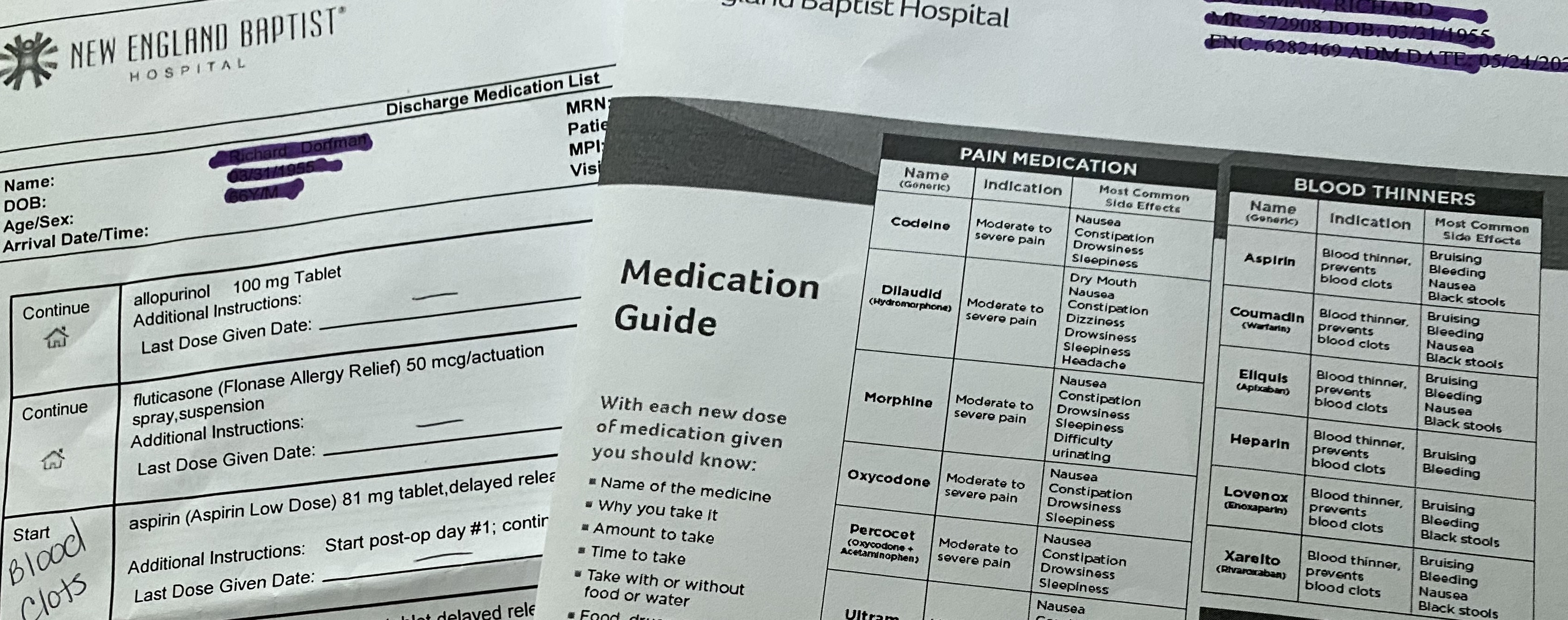 Discharge Medication informationDue to Covid, I dropped Sam off for pre-op with his crutches and cinch sack filled with paperwork and personal items for his stay. Several hours later, I was contacted by his nurse liaison about his status and about coming to his recovery room for a two- hour visit. It was not communicated to me or Sam if he would be staying over or being discharged. As 4pm neared, I asked about his discharge and the nurse moved quickly to get another PT session in to help Sam master stairs. The nurse went carefully through all discharge materials, answered all of our questions and then handed us the folder.
Discharge Medication informationDue to Covid, I dropped Sam off for pre-op with his crutches and cinch sack filled with paperwork and personal items for his stay. Several hours later, I was contacted by his nurse liaison about his status and about coming to his recovery room for a two- hour visit. It was not communicated to me or Sam if he would be staying over or being discharged. As 4pm neared, I asked about his discharge and the nurse moved quickly to get another PT session in to help Sam master stairs. The nurse went carefully through all discharge materials, answered all of our questions and then handed us the folder. - Nurse Liaison: As Sam went through pre-op, he texted me a contact card for the nurse liaison, which gave me reassurance that I had someone to connect with about his surgery status.
- What to Expect Next Discussion: Instead of just telling us what we needed to do at home, the nurse walked us through the folder at discharge, reviewing each patient education insert so we understood what to do and where to go to re-read the information. This took the pressure off of us to remember everything that was mentioned during the discharge meeting.
- What to Expect Packet/Medication: As a caregiver, I was disappointed that there were several different inserts related to medication (Med List, Medication Guide). Although it was quickly mentioned at discharge, it was not documented which medications are to be taken together (i.e. laxative with pain management meds). This would have helped us follow protocol. There also wasn’t a "medication tracking form", so as the caregiver, I had to create my own to record the times that each medication was given and indicate when medications were stopped. There is an opportunity for the provider to gather templates like this from other caregivers and provide them within the discharge packet.
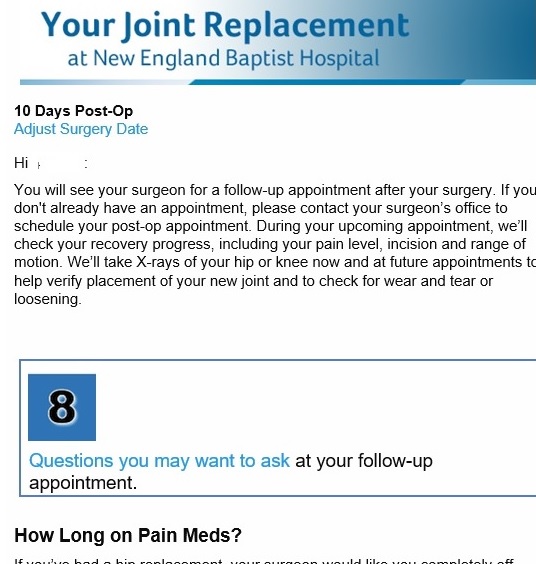 Post surgery emails tied to surgery date As promised at discharge, Sam received a call from VNA Care to schedule nurse and PT appointments. During these visits, Sam learned how he was doing, what was normal and required a call to the surgeon’s office. These visits have continued over the past few weeks, with the PT providing additional exercises for Sam to do in home.
Post surgery emails tied to surgery date As promised at discharge, Sam received a call from VNA Care to schedule nurse and PT appointments. During these visits, Sam learned how he was doing, what was normal and required a call to the surgeon’s office. These visits have continued over the past few weeks, with the PT providing additional exercises for Sam to do in home. - Care Coordination: Sam felt relieved that his care was continuous and the instructions consistent from the hospital to home, the discharge nurse to VNA Care nurse.
- Recovery perspective: Sam learned from his VNA Care nurse how he was healing relative to other patients. He felt relieved when he was able to master the PT exercises and he was off pain meds “much earlier than other patients” like him.
- Home Health Patient Education and Education Workbook: During the first VNA Care visit, the nurse handed us a 94-page book and pointed out pertinent pages for Sam and for me such as medication categorization and fall preventiion information. This helped us to not feel overwhelmed by the big workbook of information, especailly in the first few days when we are trying to address everything we need to do.
- Patient Education Journey: Sam and I find New England Baptist's post emails informative and relevent since they are tied to his surgery date and recovery milestones.
- Caregiver Post-Surgery Communication: With Sam on pain meds following surgery, it would have been helpful to have all patient communications also pushed to me/caregiver. After he was off of the pain meds and cognizant of what needed to be addressed, Sam forwarded the emails to me. I realized that several would have really been helpful such as what to look for and what to do in the first few days following surgery.
- VNA Visit Alerts: Although the nurse and PT mentioned that they were coming next Monday in the afternoon, it would have been helpful and expected for the patient and caregiver to receive a text reminder with the time range for their visit. Given that Sam is on crutches and often sitting with ice packs on his hip, I need to be available to answer the door for these visits.
- VNA Virtual Visit: As a caregiver, I had questions that needed to be addressed in between the VNA nurse visits. Although I was encouraged to call VNA Care at any time of day or night, I wished that I had the option of a virtual visit to show the nurse Sam’s swelling and bruising. This would have made me feel relieved since the nurse could have seen his hip and leg to make the best care decision instead of relying on my words to convey what I saw.